
Skin Tears! Who Cares?
Why care about skin tears? The standard for skin tear repair has always been “more is less.” The more you try primary closure with sutures, the more tissue destruction you cause, resulting in frustration and, often, a worse cosmetic result. So many, if not most, of us have just given up, taking the easy way out—“less is more”—embracing the ethical luxury of telling these patients that we have little to offer other than wound cleansing, a bio-occlusive dressing, and discharge. A quick in-and-out for you, but a poor cosmetic result and wound care hassle for them.
This old standard may have changed! Primary closure for skin tears is possible. It was never in question that primary closure of skin tears would be optimal. However, it just couldn’t be accomplished in thin-skinned patients because the sutures, no matter how small, always seemed to pull through the skin as soon as tension was applied. You can’t thicken the skin; conversation over—but not so fast. Davis et al published a paper reporting a novel technique: the use of Steri-Strips but not in the traditional sense.1 They applied Steri-Strips across the skin tear as anchoring devices and then sutured through them (see Figure 1).
After reading this article several months ago, I gave it a try. However, I modified the technique slightly due to a stellate, nonlinear wound and some tissue defect. I cut pieces of Steri-Strips for anchoring at key locations and sutured through them; my Steri-Strips did not span across the wound. My modification provided a bit more flexibility regarding the most advantageous wound edges to approximate (see Figure 2).
Oxygen Must Be Good
Oxygen is air! It is critical to survival. So how could it possibly be bad? Well, water is essential to life as well; however, too much can result in hyponatremia or even drowning (on a larger scale). A recent article by Stub reported “new” information calling the use of oxygen into question in ST segment elevation myocardial infarction (STEMI) patients who have normal oxygen saturations.2
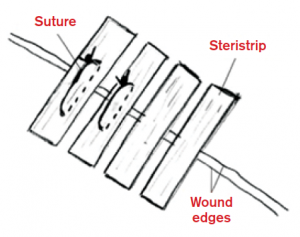
Figure 1. Davis et al applied Steri-Strips across the skin tear as anchoring devices and then sutured through them.
According to the author, “supplemental oxygen therapy in patients with STEMI but without hypoxia increased myocardial injury, recurrent myocardial infarction, and major cardiac arrhythmia, and was associated with larger myocardial infarct size assessed at six months.”
Although this article, presented at the American Heart Association Scientific Sessions in November 2014, received considerable attention, concern about the negative effects of hyperoxia is not new. The findings shouldn’t surprise us. What amazes me is that this concept is in some way a revelation. Many articles have reported this concern and have even expanded the concern to other clinical entities that are oxygen-sensitive. The surprise should be the gap between science and clinical practice.
In 1968, Brown and Hugget published this great nugget: “Oxygen at elevated pressures is known to be toxic for many forms of life. The toxicity is clearly related to both partial pressure of oxygen and the duration of exposure.”3 Although they were trying to kill bacteria with hyperoxia, they still recognized the concept that hyperoxia can be toxic.
In 1988, the effects of hyperoxia on cerebral blood flow (velocity) were actually studied. The authors reported that, “Hyperoxia has a consistent and predictable effect on cerebral blood flow in healthy adult brains.”4 Studying 15 term and 17 premature infants exposed to three times normal oxygen tension, they concluded, “The cerebral blood flow velocity fell in all 15 infants born at full term during hyperoxia, but there was a simultaneous and significant reduction in PCO2 at the same time as the hyperoxia. Analysis of variance suggested that in the infants born at full term, the change in carbon dioxide had most effect in the reduction of cerebral blood flow velocity, rather than the hyperoxia itself. We conclude that in premature infants, cerebral vascular resistance may be altered by a fall in cerebral blood flow velocity in the presence of hyperoxia.”
In 2005, coronary blood flow during left heart catheterization was studied.5 Compared to patients who received room air, patients who received 100 percent FiO2 experienced a 40 percent increase in coronary artery vascular resistance, which was accompanied by a 30 percent reduction in coronary blood flow.
A Cochrane database systematic review was performed in 2010.6 The authors identified three articles (one dating back to 1976), which encompassed 387 patients and 14 associated deaths. The relative risk for death in patients with confirmed acute myocardial infarction (AMI) who were receiving supplemental oxygen was 3.03. However, the authors admitted that the low number of reported deaths could also be attributed to chance. They noted the suggestion of harm and that no conclusive evidence exists to support the routine use of supplemental oxygen therapy in these patients. This review was updated in 2013. One additional trial was identified, increasing the total patient count to 430, with 17 deaths. The conclusions were unchanged, including a call to action for a more definitive study.
In 2012, Cornet et al published an excellent systematic review on oxygen administration in emergencies.7 They concluded that the outcomes in many disease entities are worsened by supplemental oxygen administration. Many conditions are worsened by the use of supplemental oxygen in patients without hypoxia: these include AMI, congestive heart failure, chronic obstructive pulmonary disease, and stroke.

Figure 2. For my modification, I cut pieces of Steri-Strips for anchoring at key locations and sutured through them. Note that tissue loss and defect and significant tension did not allow for approximation of all wound edges.
Now, back to AVOID (Air Versus Oxygen In ST-elevation MyocarDial Infarction). Perhaps this is the trial that the Cochrane crew was looking for. In it, 638 patients with suspected STEMI (441 confirmed) were randomized to no oxygen (unless SaO2 <94%) or 8 L/min via simple face mask. The primary end point was infarct size (good choice), but the measure of infarct size was total creatine phosphokinase (CPK) and troponin I (surrogate markers). Biomarkers do predict AMI, but their ability to accurately predict infarct size has been challenged.8 A redeeming feature of the study was the confirmation of increased myocardial damage at six months via cardiac MRI.
Other limitations include the use of 8 L/min oxygen for the treatment group. In general, 2–4 L/minute via cannula is more consistent with current U.S. practice. Finally, we have to recognize the limitation of pulse oximetry. Using pulse oximetry to estimate actual arterial oxygen tensions (I’m not suggesting the use of arterial blood gases) is akin to using bifocals to pick up a grain of salt. For instance, a pulse oximetry range between 92 percent and 96 percent will likely have a much larger range of arterial oxygen tension associated with it. The vasoactive effect that oxygen has on chemoreceptors is a microscopic phenomenon.
Despite the fact this study, and many before it, have had limitations, we have forgotten one thing—common sense. I think we can stop studying this concept. Although perhaps the scientist in all of us longs for that one definitive study, we are victims of paralysis by analysis. We have enough evidence to conclude that giving this drug to people without a demonstrated need (eg, hypoxia) provides them no benefit and may, in fact, cause harm.
Oxygen is a vasoactive drug. This is an indisputable fact. Give this drug to patients who don’t need it, and whether you can prove it with scientific rigor or not, you will eventually hurt people.
Alcohol Levels: What Question Are You Asking?
Some tests have their utility stretched beyond rational use. Blood alcohol levels are frequently ordered but have limited clinical value, and such ordering patterns are validated and encouraged with positive results. I think we have collectively forgotten what questions we need to ask and what the right test(s) is to find those answers. Alcohol levels may be important when we are determining the source of an altered mental status, but when the source is clear, why order it? For instance, a negative ethanol level in a patient with minor head trauma should point the diagnostic compass immediately toward intracranial injury, but when patients say they drank a six-pack, you can smell it, and they appear intoxicated, does your laboratory really need to confirm the presence of alcohol? If confirmation is warranted, why not a breathalyzer? If you say you’re drunk, your breath says you’re drunk, and I think you’re drunk, you’re drunk.
OK, so the patient is drunk. Some then might say that the blood alcohol level is obtained to determine the level of intoxication. I honestly believe that the term “blood alcohol level” almost implies a correlation between intoxication and the number (level). We know that the effects of alcohol are very idiosyncratic; everyone experiences a different response based on a multitude of factors, including their level of exposure, comorbidities, previous exposure, etc. Historically, we believed that the number could be applied to a formula to predict clearance. This has been disproved. Furthermore, Roberts and Dollard published an article in 2010, and the conclusions are words to live by: “Attempting to relate observed signs of alcohol intoxication or impairment, or to evaluate sobriety, by quantifying blood alcohol levels can be misleading, if not impossible.”9
The only reliable test for determining the level, or degree, of intoxication is the physical examination. In other words, if you can carry on a normal conversation, your judgment and insight are reasonable, and your motor function is not impaired (eg, ambulation without difficulty, no slurred speech), you’re not clinically intoxicated. Having all of the providers agree to this assessment in the medical record is key to avoiding discrepancies. However, adding an unnecessary blood alcohol level into the diagnostic picture only serves to cast doubt on your clinical determination that the patient wasn’t impaired. Impairment is the key, not a specific number. Remember, the legal level of intoxication (different from state to state) relates to a person’s ability to legally operate a motor vehicle in that state. This arbitrary level has no clinical basis and should not be applied in the world of clinical medicine.
Unnecessary blood alcohol levels in the medical record may cast doubt on your clinical assessment and may obviate you to observe your patients for extended periods of time while waiting for them to achieve a level for safe motor vehicle operation in your state, a number irrelevant to the clinical management of your patient.
 Dr. Klauer is the chief medical officer-emergency medicine and chief risk officer for TeamHealth as well as the executive director of the TeamHealth Patient Safety Organization. He is an assistant clinical professor at Michigan State University College of Osteopathic Medicine; Speaker of the ACEP Council; and medical editor in chief of ACEP Now.
Dr. Klauer is the chief medical officer-emergency medicine and chief risk officer for TeamHealth as well as the executive director of the TeamHealth Patient Safety Organization. He is an assistant clinical professor at Michigan State University College of Osteopathic Medicine; Speaker of the ACEP Council; and medical editor in chief of ACEP Now.
References
- Davis M, Nakhdjevani A, Lidder S. Suture/Steri-Strip combination for the management of lacerations in thin-skinned individuals. J Emerg Med. 2011;40:322-3.
- Stub D. A randomized controlled trial of oxygen therapy in acute ST-segment elevation myocardial infarction: the Air Versus Oxygen in Myocardial Infarction (AVOID) study. Presented at: American Heart Association Scientific Sessions; Nov. 19, 2014; Chicago, IL.
- Brown OR, Huggett DO. Effects of hyperoxia upon microorganisms. Appl Microbiol. 1968;6:476-9.
- Niijima S, Shortland DB, Levene MI, Evans DH. Transient hyperoxia and cerebral blood flow velocity in infants born prematurely and at full term. Arch Dis Child. 1988;63:1126-30.
- McNulty PH, King N, Scott S, et al. Effects of supplemental oxygen administration on coronary blood flow in patients undergoing cardiac catheterization. Am J Physiol Heart Circ Physiol. 2005;288:H1057-62.
- Cabello JB, Burls A, Emparanza JI, et al. Oxygen therapy for acute myocardial infarction. Cochrane Database Syst Rev. 2010;(6):CD007160.
- Cornet AD, Kooter AJ, Peters MJ, et al. Supplemental oxygen therapy in medical emergencies: more harm than benefit? Arch Intern Med. 2012;172:289-90.
- Arruda-Olson AM, Roger VL, Jaffe AS, et al. Troponin T levels and infarct size by SPECT myocardial perfusion imaging. JACC Cardiovasc Imaging. 2011;4:523-533.
- Roberts JR, Dollard D. Alcohol levels do not accurately predict physical or mental impairment in ethanol-tolerant subjects: relevance to emergency medicine and dram shop laws. J Med Toxicol. 2010;6:438-42.







2 Responses to “Sutures for Skin Tears, Oxygen Therapy for STEMI Patients, and Blood Alcohol Levels to Assess Intoxication: More Myths in Emergency Medicine”
February 8, 2015
Derek McCalmontDr. Klauer incorrectly states that the level of blood alcohol for legal intoxication varies from state to state. Laws and penalties vary but the level of .08 is universal across all 50 states.
At what point does Dr. Klauer propose discharge for intoxicated patients without family or friends to assume care in the absence of a blood alcohol level?
February 19, 2015
suture through Steri-strips | DAILYEM[…] ACEP Now article + pictures; original 2011 article for idea […]