The emergency department serves as both the lifeline and the gateway to psychiatric care for millions of patients suffering from acute behavioral or mental health emergencies. As ED providers, in addition to assessing the risk of suicide and homicide, one of our most important responsibilities is to determine whether the patient’s behavioral emergency is the result of an organic disease process, as opposed to a psychological one; there is no standard process for this.
Explore This Issue
ACEP Now: Vol 36 – No 09 – September 2017On the one hand, these psychiatric patients are high-risk medical patients. They not only have a higher incidence of chronic medical conditions, but they’re at greater risk of injury, including serious head injury, than the general population. The rate of missed medical diagnoses in the emergency department ranges from 8 to 48 percent, with the highest missed diagnosis rate among first presentations. Any and all acute medical emergencies need to be identified. The admitting psychiatric team certainly shouldn’t be burdened with a missed medical emergency.
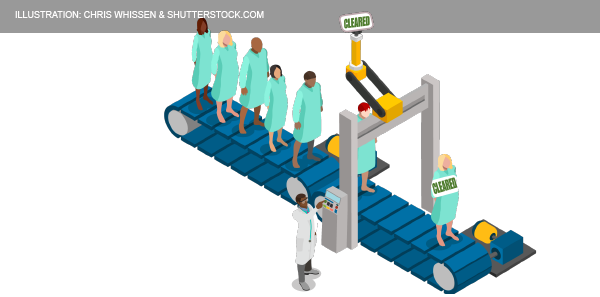
On the other hand, psychiatric patients can stress the emergency department, with the average length of stay ranging from 15 to 30 hours, depending on the whether they require medical clearance and whether they are admitted.1,2 Lack of agreement between the emergency department and the psychiatric department can lead to the adoption of arbitrary exclusionary criteria, which delay admissions even further. In one study, the total costs were $17,240 per patient requiring medical screening.3 So, having these patients who are at high risk for acute medical problems that need to be dealt with before their disposition while at the same time wanting to move them through the system efficiently poses significant challenges. An appropriate and accurate medical clearance process is imperative for decreasing length of stay in the emergency department and the cost of care as well as for identifying medical issues that may be causing or exacerbating the patients’ presentation.
General Approach to Behavioral Complaints
Overall, the approach to patients presenting with behavioral complaints should be the same as the approach to those with general medical conditions: ABCs, a thorough history (including collateral history) and physical, and selective testing.
History and physical exam remain the mainstays of evaluation; the minimum data set should include full vital signs, history including record of mental illness, medications, substances, mood and thought content, mental status exam, and further examination as indicated by the presentation. In a 1997 study by Olshaker et al of 345 patients presenting to an emergency department with psychiatric complaints, a complete history was the most sensitive, at 94 percent, for identifying a common medical condition compared to physical and lab tests.4 If you are unable to obtain a history from an altered patient, the risk for missing an important medical illness goes up significantly.
Historical Clues to Differentiate Organic Versus Psychiatric Illness
Patients who present with an altered level of awareness or a dramatic change in behavior often end up getting extensive and expensive workups that could be avoided by asking them a few simple questions: Where do you live? Who do you live with? How do you support yourself? Do you have any outstanding charges you’re facing? Have you ever been in jail? What substances do you regularly use? Where were you just before you came to the emergency department?
Several factors favor psychiatric illness including history of psychiatric illness, younger age, and onset over weeks to months. Factors favoring organic illness include no history of psychiatric illness, age older than 40 years, onset over hours to days, complaint of headache, and any recent new medication.5
A detailed extensive mental status exam is not necessary in every patient with a behavioral problem. A study in the American Journal of Emergency Medicine showed that the Quick Confusion Scale is as reliable as a full Mini-Mental Status Examination in revealing an altered level of awareness that may help pick up organic pathology.6
The three key elements of the mental status exam are orientation, memory, and judgment, which can often be gleaned from the patient encounter by an experienced EM provider without using a validated scale.
Generally speaking, auditory hallucinations are more indicative of a psychiatric illness, whereas visual hallucinations are more indicative of an organic illness. While about 15 percent of patients with schizophrenia are said to experience visual hallucinations, these tend to occur in those schizophrenics with severe illness and usually in addition to auditory hallucinations.
Physical Exam Clues to Differentiate Organic Versus Psychiatric Illness
As always, vital signs are vital! Any abnormality in vital signs should be addressed and accounted for.
Hypoglycemia can mimic many psychiatric illnesses, from catatonic schizophrenia to severe depression, and could be considered as “the sixth vital sign”: blood glucose (ABC Don’t Ever Forget Glucose).
Look for fluctuating level of awareness as it is rare in isolated psychiatric illness and often signifies delirium with an underlying toxin, metabolic abnormality, or central nervous system lesions. Scrutinize the patient’s eyes. Any abnormality in gaze, nystagmus, pupillary dilation, etc. may signify organic pathology. Ask the patient to protrude their tongue. If you see a laceration, think about a postictal state. Take a moment to look up the patient’s nose; you might be surprised to find cocaine, crushed bupropion, or any number of toxins that the patient has insufflated.
Screening Lab Tests or Head CT Scan?
There is no evidence-based list or panel of investigations or order set that can be applied to all psychiatric patients requiring medical clearance.
Routine lab test screening: Several retrospective studies suggest that for psychiatric patients presenting to the emergency department with a behavioral chief complaint, almost all acute medical illnesses requiring treatment could have been identified if a thorough history and physical were performed and that routine laboratory screening has a very low yield for clinically significant acute medical illness.7-9
Urine drug screens are not required routinely in the psychiatric patients, as supported by the ACEP guidelines. Most patients, if asked in a nonaccusatory manner, will tell you what drugs they have recently taken. Olshaker et al found that the reliability of self-reported drug use had a sensitivity of 92 percent and specificity of 91 percent.4 The reliability of self-reported alcohol use was 96 percent sensitive and 87 percent specific. In addition, urine drug screens have many false positives and negatives, which can be misleading.
Literature suggests a very low rate of clinically significant imaging findings in psychiatric patients without risk factors for organic illness. The yield of a clinically significant finding on a CT of the head in uncomplicated schizophrenia patients with normal vital signs and an otherwise normal physical exam (even if it is a first-time presentation) was published in a Canadian Journal of Emergency Medicine study.10 From three Ontario hospitals, the yield was one in 300. Another review of five studies from 2009 showed the diagnostic yield to be only 1.3 percent for CTs and 1.1 percent for MRIs in 384 CTs and 184 MRIs of first episode psychosis patients. CT is clinically indicated in psychiatric patients with altered mental status, trauma, immunodeficiency, or focal neurological findings.
Three Main Take-Home Points in Medical Clearance
- Approach to psychiatric patients should be the same as your approach to any medical patient. An adequate history and physical are essential.
- Know which patients are at high risk for an organic cause of their behavioral presentation so that you have a heightened awareness for organic pathology in these patients.
- There is no evidence for benefit of routine diagnostic screening; tests should be ordered just as you would for medical patients, guided by the presenting complaint and findings on a thorough history and physical examination.
Thanks to Howard Ovens, Ian Dawe, and Brian Steinhart for their expert contributions to the EM Cases podcast that inspired this article.
 Dr. Helman is an emergency physician at North York General Hospital in Toronto. He is an assistant professor at the University of Toronto, Division of Emergency Medicine, and the education innovation lead at the Schwartz/Reisman Emergency Medicine Institute. He is the founder and host of Emergency Medicine Cases podcast and website.
Dr. Helman is an emergency physician at North York General Hospital in Toronto. He is an assistant professor at the University of Toronto, Division of Emergency Medicine, and the education innovation lead at the Schwartz/Reisman Emergency Medicine Institute. He is the founder and host of Emergency Medicine Cases podcast and website.
References
- Zhu JM, Singhal A, Hsia RY. Emergency department length-of-stay for psychiatric visits was significantly longer than for nonpsychiatric visits, 2002-11. Health Aff (Millwood). 2016;35(9):1698-706.
- Weiss AP, Chang G, Rauch SL, et al. Patient- and practice-related determinants of emergency department length of stay for patients with psychiatric illness. Ann Emerg Med. 2012;60(2):162-71.e5.
- Santillanes G, Donofrio JJ, Lam CN, et al. Is medical clearance necessary for pediatric psychiatric patients? J Emerg Med. 2014;46(6):800-807.
- Olshaker JS, Browne B, Jerrard DA, et al. Medical clearance and screening of psychiatric patients in the emergency department. Acad Emerg Med. 1997;4(2):124-128.
- Janiak BD, Atteberry S. Medical clearance of the psychiatric patient in the emergency department. J Emerg Med. 2012;43(5):866-870.
- Huff JS, Farace E, Brady WJ, et al. The quick confusion scale in the ED: comparison with the mini-mental state examination. Am J Emerg Med. 2001;19(6):461-464.
- Donofrio JJ, Santillanes G, McCammack BD, et al. Clinical utility of screening laboratory tests in pediatric psychiatric patients presenting to the emergency department for medical clearance. Ann Emerg Med. 2014;63(6):666-675.e3.
- Amin M, Wang J. Routine laboratory testing to evaluate for medical illness in psychiatric patients in the emergency department is largely unrevealing. West J Emerg Med. 2009;10(2):97-100.
- Shihabuddin BS, Hack CM, Sivitz AB. Role of urine drug screening in the medical clearance of pediatric psychiatric patients: is there one? Pediatr Emerg Care. 2013;29(8):903-906.
- Ng P, McGowan M, Steinhart B. CT head scans yield no relevant findings in patients presenting to the emergency department with bizarre behavior. CJEM. 2016;18 Suppl 1:S50.
Pages: 1 2 3 4 | Multi-Page





No Responses to “How to Tell Whether a Psychiatric Emergency is Due to Disease or Psychological Illness”