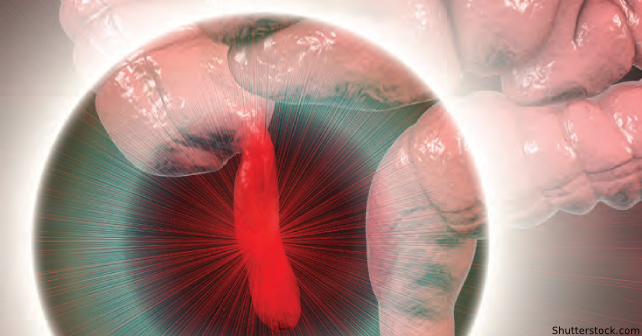
In 2020, following publication of the Comparison of Outcomes of Antibiotic Drugs and Appendectomy (CODA) trial, the largest randomized controlled trial of antibiotics versus urgent appendectomy for uncomplicated appendicitis (i.e., localized, no abscess or diffuse peritonitis), the American College of Surgeons issued guidelines stating that high-quality evidence existed supporting that most patients with appendicitis can be treated nonoperatively, with antibiotics, rating this as a first-line alternative to surgery.1,2 One unique aspect of the CODA trial was that patients randomized to antibiotics—following receipt of initial parenteral antibiotics—could be discharged from the emergency department (ED) for outpatient management on oral antibiotics if they met stability criteria and the patient and their doctor were comfortable with this plan.
Explore This Issue
ACEP Now: Vol 41 – No 12 – December 2022In July, we published the results of a secondary analysis of the CODA trial comparing outcomes among 335 participants getting outpatient care and 391 who were hospitalized, which supported the safety of outpatient management.3 Through seven days, outpatient care tended to be associated with fewer serious adverse events (0.9 versus 1.3 per 100; no deaths occurred) and appendectomies (9.9 percent versus 14.1 percent) than in-hospital care, even when adjusted for illness severity factors. Those discharged from the ED had no more return visits and missed one day less of work, at 2.6 days (the CODA trial found nine disability days with routine appendectomy).1
Avoiding hospitalization and surgery leads to better patient convenience, productivity, and substantially reduced direct medical and patient out-of-pocket costs. But, considering that appendicitis has been an easy automatic hospital admission and the legacy of the now disproven appendix-burst-kill-you narrative, will emergency physicians feel comfortable discharging an appendicitis patient like we routinely do for acute diverticulitis (not getting into whether that needs antibiotics or not)? I see some barriers:
- Surgeon says “No”—Not so surprisingly, doing surgery is still popular among surgeons. However, surveys show most people would prefer to avoid surgery even if the appendicitis recurrence rate was as high as 60 percent.4 Excluding elective appendectomies, probably the chance of a true recurrence is about 20 percent and only through about one year, and retreatment with antibiotics is effective.5 Although it’s our patient in the ED, we’re not quite at a place yet where a surgeon would not be consulted, and it’s nice to stay on good terms with the medical staff who bring the most money into the medical center. However, more surgeons are coming around to offering this approach, especially after hours or on the weekend.
- I Could Be Sued—Evidence and guidelines from U.S. and international surgical societies back up the medical decision making to use antibiotics only for acute appendicitis, but let’s face it, it’s hard to shake off 120 years of a disease being viewed as a ticking time bomb requiring emergency surgery. Interestingly, rupture is observed at operation less frequently among those treated with antibiotics. Operations more extensive than a routine appendectomy are not required more frequently among those getting antibiotics. And surgeons who do not at least offer nonoperative treatment are now at medical-legal risk should a patient have a surgical complication.
- It’s Easier to Admit the Patient—Perhaps you can recall the halcyon days when hospital admission from the ED was easy. Now, hospitals are overfilled and staffing is in short supply, and ED beds are cannibalized by boarders. Yes, you have to observe the patient, control their pain and nausea, and give them at least a dose of ertapenem or ceftriaxone and high-dose metronidazole (1,500 mg) before discharging on cefdinir and metronidazole for seven to 10 days. On the other hand, this can all happen while you are awaiting labs and imaging findings, and running things by your surgeon friend, which you have to do anyway. And no specialist is a better judge of “sick/not sick” and of who can go home than emergency physicians.
- Who Follows Up?—Having treated many appendicitis patients as outpatients myself, both through research studies and in the course of regular care, I’ve found the usual discharge instructions, like you’d give diverticulitis patients (come back if worse), and a follow-up telephone call at 24–48 hours is sufficient. Patients who respond do so within 48 hours, otherwise they should return for reevaluation. But who does it? At one hospital I worked, we have a nurse telephone follow-up service. Sometimes the surgeon on call will have their office call or have a follow-up appointment made. And other times, the patient’s general physician is contacted, and some are now familiar and comfortable with this treatment approach.
Treatments That Work?
Is the outpatient antibiotic treatment of appendicitis a “paradigm shift”?6 I suspect it will be more drift than shift. Patients in the ED are our patients first. We educate them about their diagnosis, but now can also introduce them to two safe treatment options with different advantages. Surgery—a permanent solution requiring general anesthesia, laparoscopic surgery, one day in the hospital, and at least a week’s recovery. Antibiotics—most patients will avoid surgery altogether and get on their feet days sooner, at less cost but with a chance of recurrence. This new study shows that most appendicitis patients will be stable enough to be discharged from the ED and cure their case of appendicitis while comfortably at home.
 Dr. Talan is emeritus professor of emergency medicine and medicine/infectious diseases at the David Geffen School of Medicine at UCLA in Los Angeles.
Dr. Talan is emeritus professor of emergency medicine and medicine/infectious diseases at the David Geffen School of Medicine at UCLA in Los Angeles.
References
- The CODA Collaborative. A randomized trial comparing antibiotics and appendectomy for appendicitis. N Engl J Med. 2020;383:1907–19.
- American College of Surgeons. COVID-19 guidelines for triage of emergency general surgery patients. Updated December 8, 2020. Available at: https://www.facs.org/covid-19/clinical-guidance/elective-case/emergency-surgery. Accessed October 11, 2022.
- Talan DA, Moran GJ, Krishnadasan A, et al. The CODA collaborative. Analysis of outcomes associated with outpatient management of nonoperativelytreated patients with appendicitis. JAMA Netw Open. 2022;5(7):e2220039.
- Rosen JE, Agrawal N, Flum DR, et al. Willingness to undergo antibiotic treatment of acute appendicitis based on risk of treatment failure. Br J Surg. 2021;108:e361–e363.
- Newdow M. Management of acute appendicitis – longer-term outcomes. N Engl J Med. 2022;386:900.
- Hamza Z. Antibiotics safe for some outpatients with acute appendicitis – secondary analysis of the CODA trial showed no greater risk of complicating or appendectomy. MedPageToday website. Available at: https://www.medpagetoday.com/gastroenterology/generalgastroenterology/99573. Published July 5, 2022. Accessed October 11, 2022.
Pages: 1 2 | Multi-Page




No Responses to “The Future of Antibiotics and Appendicitis in the Emergency Department”