
There is a debate going on in the inpatient world among hospitalists, bed management and other hospital leaders and managers. It is one that emergency physicians should familiarize themselves with because it affects hospital-wide patient flow and thereby boarding in the emergency department (ED). It involves hospitalist medicine, which is now the largest admitting service at most hospitals and the service that the emergency physician interfaces with most often. The debate is whether hospitalists should work in geographic zones in the hospital. You may hear it discussed using a number of terms including geographic localization, geographic rounding, geographic cohorting, or simply geography. These terms refer to the placement of patients on a physician’s service into a defined area, typically a unit or a floor, as opposed to distributing them throughout the hospital.
Explore This Issue
ACEP Now: Vol 41 – No 04 – April 2022In the late 1990s, geography was a promising strategy for hospitalist medicine.1 Geography allows the health care team (physician, APP, nurse, physical therapist, case manager) to work all together in proximity to their patients. It improves communication, improves productivity, removes wasted time spent in transit and improves length of stay by facilitating the discharge process.2 As servers in the hospitality industry discovered, it is much more efficient for waitstaff to have all their tables in one area. Most nurses, (whether working on an inpatient unit or in the emergency department), have assignments involving contiguous rooms. Hospitalists found similar advantages when working on one hospital unit or floor.
However, in the 2000s, after many hospital closures, hospital bed occupancy rates became higher and bed capacity was tight. Many hospitalist services gave up geographic localization and patients were now assigned to whatever staffed bed was available. At the same time, there was a growing concern in health care for the hand-off of patients. Consequently, patients were no longer re-distributed after admission to be cared for by a single physician staffing a unit. Hospitalists now had patients scattered all over the hospital, covering massive inpatient footprints. Insidiously, as they abandoned the concept of geography, they found themselves caring for patients on many different floors (often in many different towers). The walk between patients situated in the farthest points of the hospital might exceed 20 minutes!
Meanwhile, the rest of the care team (nurses and case managers) continued to work in a unit-based or floor-based model. The care team became fragmented, and communication faulty. Facts about a patient’s care and course that were small but consequential were not shared in a systematic manner. Traditional rounding with the entire care team was often abandoned. Today’s hospitalized patients are increasingly complex, and there are many necessary interfaces between care team members, subspecialists and families during the hospital stay. Robust and regular communication has become essential to optimize patient care. Thus, the fractured care team suffers from lapses in communication resulting in delays and dangers to patient care. Patients often experience discharge delays that are the result of these communication breakdowns, resulting in longer inpatient stays.
In one study surveying hospitalists, 85 percent reported geographic localization and rounding was the most efficient care model.3 Studies have shown that when patients are situated in proximity to their care team members, communication is improved, and this translates into improvements in length of stay and decreased total rounding time.4 Geographic localization increased the direct communication between members of the care team and increased the likelihood that these team members could correctly identify one another.5 When residents have geographic localization, the number of rapid response calls goes down.6 Further, geographic localization was viewed to have a positive effect on the resident experience.7
Geographic Localization Pro’s
- Better communication among patient care team
- Saves time
- Quick service to patient
- Better HCAHPS scores
- Shorter LOS
- Lower readmission rates
- Reduction in sentinel events
- Reduced time on round
- Higher resident satisfaction at teaching hospitals
Geographic Localization Con’s
- Too many hand-offs
- Interruptions on work rounds
- Load leveling is difficult
- Stationary work environment
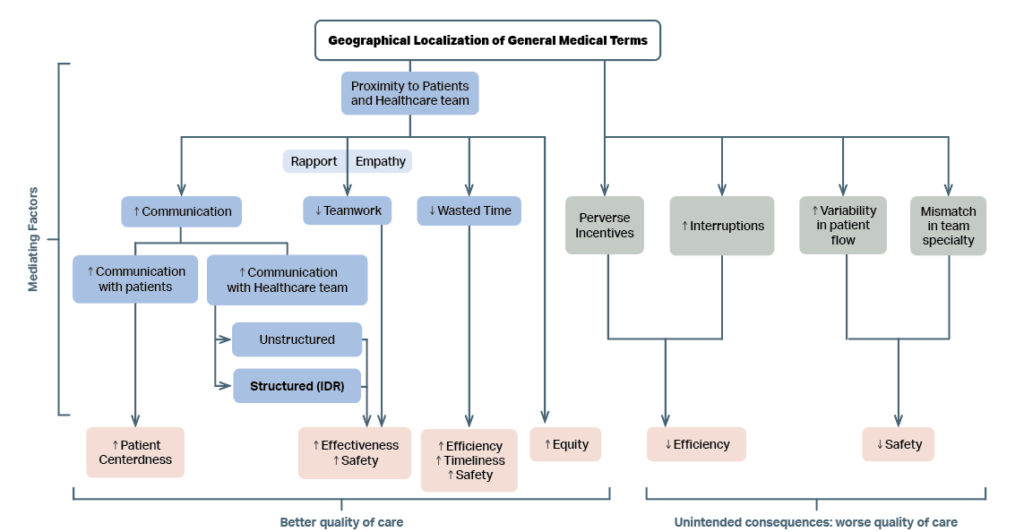
The Medical College of Wisconsin reported the responses of their faculty and nurses to the introduction of geographic localization.8 Figure 1 shows the response to the initiative.
(click for larger image)
FIGURE 1: Conceptual model depicting impact of geographical localization of general medical teams on quality of care. Mediating factors that lead to better quality of care are described in blue boxes. Mediating factors that are unintended and lead to worsening quality of care are described in grey boxes. The impact on domains of quality of care is described in pink boxes. ‘↑’ indicates an increase; ‘↓’ indicates a decrease; IDR = Interdisciplinary Rounds.
Singh S, Fletcher KE. A qualitative evaluation of geographical localization of hospitalists: how unintended consequences may impact quality. J Gen Intern Med. 2014;29(7):1009-1016.
Geographic localization has been coupled with another innovation: separating the admitting role and the rounding role for hospitalists. Thus, the “triagist” role was born: One hospitalist will admit a patient (the triagist), while another subsequently manages care. Separating these roles improved efficiency and throughput.9 The triagist role allows the patient to be admitted in a timely fashion, and placed on the right unit and team later on. Another related improvement has been the multidisciplinary rounds, particularly those that focus on the discharge of the patient. Geography makes those team rounds more feasible. 10
Another strategy which optimizes hospital throughput involves adjusting the work schedules of hospitalists.11 Schedules that promote continuity were associated with lower mortality, lower readmission rates, higher rates of discharge to home and lower 30-day post discharge Medicare costs.12-13
Strategies that help reduce hospital length of stay and improve discharge efficiency and ultimately reduce boarding in the emergency department. Emergency physicians know first-hand the advantages in communication and workflow as most of us work in designated zones and lead care teams dedicated to the patients placed in a particular geographic area.
When hospitalists consider the “geography” question, we can bring an understanding of the issue both in the inpatient and ED universes. Supporting geographic localization strategy helps improve inpatient throughput help create open inpatient beds. And open beds are the only solution to the problem of emergency department boarding!
DR. WELCH has been a practicing emergency physician for over thirty years. She has written numerous articles and three books on ED quality, safety, and efficiency. She is a consultant with Quality Matters Consulting, and her expertise is in ED operations.
DR. VASQUEZ is an Assistant Professor of Medicine at Emory University. of Operations for the Division of Hospitalist Medicine at Emory. He writes a Hospitalist Medicine Blog focused on operational excellence.
References
- Bryson C, Boynton G, Stepczynski A ,et al. Geographical assignment of hospitalists in an urban teaching hospital: feasibility and impact on efficiency and provider satisfaction. Hosp Pract (1995). 2017;45(4):135-142.
- Singh S, Tarima S, Rana V, et al. Impact of localizing general medical teams to a single nursing unit. J Hosp Med. 2012;7(7):551-556.
- Mirabella AC, McAmis NE, Kiassat C, et al. Preferences to improve rounding efficiency amongst hospitalist: a survey analysis. J Community Hosp Intern Med Perspect. 2021;11(4):501-506. Mirabella AC, McAmis NE, Kiassat C, et al. Preferences to improve rounding efficiency amongst hospitalist: a survey analysis. J Community Hosp Intern Med Perspect. 2021;11(4):501-506.
- Huang KTL, Minahan J, Brita-Rossi P, et al. All together now: impact of a regionalization and bedside rounding initiative on the efficiency and inclusiveness of clinical rounds. J Hosp Med. 2017;12(3):150-156.
- O’Leary KJ, Wayne DB, Landler MP, et al. Impact of localizing physicians to hospital units on nurse-physician communication and agreement on the plan of care. J Gen Intern Med. 2009;24(11):1223-1227.
- Williams A, DeMott C, Whicker S, et al. The impact of resident geographic rounding on rapid responses. J Gen Intern Med. 2019;34(7):1077-1078.
- Klein AJ, Veet C, Lu A, et al. The effect of geographic cohorting of inpatient teaching services on patient outcomes and resident experience [published online ahead of print January 24, 2022]. J Gen Intern Med.
- Singh S, Fletcher KE. A qualitative evaluation of geographical localization of hospitalists: how unintended consequences may impact quality. J Gen Intern Med. 2014;29(7):1009-1016.
- Coates E, Quisenberry E, Williams B, et al. Focusing hospitalist roles on either admitting or rounding facilitates unit-based assignment and is associated with improved discharge efficiency. Hosp Pract (1995). 2021;49(5):371-375.
- Ibrahim H, Harhara T, Athar S, Nair SC, Kamour AM. Multi-Disciplinary Discharge Coordination Team to Overcome Discharge Barriers and Address the Risk of Delayed Discharges. Risk Manag Healthc Policy. 2022 Feb 2;15:141-149.
- Wells M, Coates E, Williams B, et al. Restructuring hospitalist work schedules to improve care timeliness and efficiency. BMJ Open Qual. 2017;6(2):e000028.
- van Walraven C. The influence of hospitalist continuity on the likelihood of patient discharge in general medicine patients. J Hosp Med. 2018;13(10):692-694.
- Goodwin JS, Shuang Li, Yong-Fang K. Association of the work schedules of hospitalists with patient outcomes of hospitalization. JAMA Intern Med. 2020;180(2):215-222.
Pages: 1 2 3 | Multi-Page





No Responses to “The Hospital Geographic Zone Debate Pendulum Is Swinging Back”