In 2020, New Mexico established the New Mexico (NM) Bridge—a new initiative to address the state’s rapidly rising opioid-overdose death rate. The NM Bridge partners with hospitals across New Mexico to initiate emergency department (ED) and hospital-based medication for opioid use disorder (MOUD) programs while assuring linkage to community treatment. MOUD programs improve long-term recovery and reduce risk of death by combining FDA-approved drugs with behavioral therapies for people diagnosed with opioid use disorder (OUD).1,2 Brief intervention and facilitated referral to community-based treatment services is much needed in NM where the opioid overdose rate exceeds the national average, with overdoses reaching an all-time high in 2021 due to illicit fentanyl and exacerbated by the COVID-19 pandemic.3 This is particularly concerning in NM, which is the fifth-largest state in the U.S. by land mass, is highly rural and poor, and has persistent behavioral-health workforce shortages.4,5 We describe how NM Bridge partnered with rural hospitals to expand access for OUD treatment and behavioral-health workforce across a highly rural state with limited services.
Explore This Issue
ACEP Now: Vol 42 – No 03 – March 2023Multifaceted State Response
NM has significant need for OUD treatment, but an inadequate supply of prescribing clinicians.5 To address high rates of opioid use and overdose, the state tripled spending and enacted significant policy changes to expand substance-use disorder (SUD) treatment providers, treatment, and harm-reduction strategies.6 Yet, the number of prescribers remains low, particularly in rural NM. To address this, the state’s Behavioral Health Service Division allocated funding from the State Opioid Response (SOR) grant to establish the NM Bridge Program. NM Bridge focuses on training hospital physicians and nurses to identify and immediately treat patients using medications (e.g., buprenorphine) for opioid treatment in EDs and helping hospitals establish outpatient follow-up at time of discharge. As rural communities generally lack health care services, the local hospital is a primary treatment location.7 Thus, NM Bridge’s focus on expanding prescribers in rural hospitals has an outsized impact on access to medication-based OUD treatment in these communities.
Medication for Opioid Use Disorder from the ED
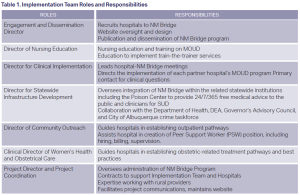
Core to the NM Bridge program is the implementation team, whose members have complementary knowledge within emergency medicine, primary care, addiction medicine, medical toxicology, billing/Medicaid reimbursement, nursing education, rural health, and peer support. Importantly, the majority of team members have expertise in providing care and implementing best treatment practices with rural clinicians. (Table 1). The implementation team guides partner hospitals from start to finish in establishing their ED-based MOUD program. The team engages other hospital units (e.g., inpatient and obstetrics) and establishes outpatient follow-up pathways for continued treatment with medication and therapy. Additionally, the NM Bridge established a 24/7 addiction-medicine consult service through the NM Poison Center, available to any clinician in New Mexico.
The NM Bridge Process
Engaged hospitals were eligible for one year of funding to support the hospital and clinicians in establishing ED-based MOUD programs. Funding covered clinical time, educational opportunities, and trainings. One year of salary was available for a peer-support worker or social worker to link the patient to treatment in the community, improving follow-up.8
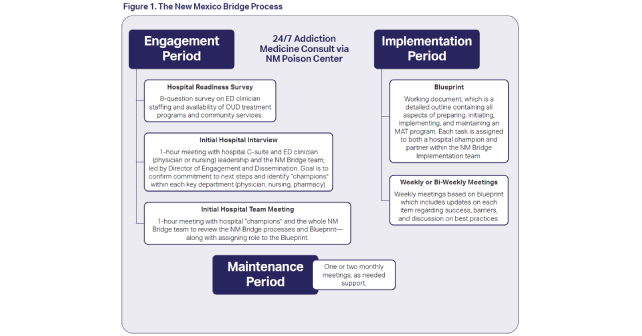
The NM Bridge process has three stages: engagement, implementation, and maintenance periods (Figure 1). Engagement focuses on initial outreach and confirmation of a hospital’s commitment to the program. Engaged hospitals demonstrate their commitment by completing an initial survey to identify current resources and gaps in care, assembling a team of champions including representatives from emergency physicians, nursing, social work, pharmacy, inpatient, and outpatient (Table 2), and submitting a budget to the Behavioral Health Service Division. In the implementation period, the implementation team and the hospital’s champions meet weekly, aligning their work to the NM Bridge’s blueprint (Table 3). During the maintenance phase, meetings typically move to once monthly, with the option to meet more often as needed to address any issues as they arise.
Addressing Rural Disparities
The NM Bridge is designed to increase the number of prescribers and hospital staff who can treat OUD, increasing access to these services in rural New Mexico. Rural communities in NM face the highest rates of OUD overdose, which is increasingly impacting indigenous communities and rates are disproportionately high among the American Indian/Alaska Native (AI/AN).3,9 Implementing MOUD programs at rural hospitals is challenging due to limited workforce, a lack of dedicated personnel for quality improvement, thin financial margins, and OUD-related stigma. NM Bridge addresses all of these barriers by supporting rural hospitals with a dedicated team using a hands-on approach of MOUD implementation with financial support and robust training.
Grant support is key and brings needed resources to rural hospitals. This includes the implementation team’s expertise, along with financing to hire a peer-support position or a social worker and to cover clinician and staff education time. Trainings address stigma and education across all clinician groups and are designed for the rural context. Through weekly meetings and hands-on partnership, the implementation team directly facilitates the local hospital’s implementation. As the rural outpatient ecosystem is fragile, a critical aspect of the program is assuring continued MOUD following ED or hospital discharge. The clinic/outpatient champion role is designed to address this rural-specific consideration by confirming outpatient follow-up. Further, hospitals identify a backup, community-based, OUD treatment program, and at minimum establish a relationship with a telemedicine service.
The maintenance period of the program brings an ongoing support system and 24/7 access to addiction-medicine consultation for difficult cases. The funding, training, comprehensive team approach, and the ongoing support makes NM Bridge effective in the rural space. Other largely rural states may wish to follow New Mexico’s lead, using (or applying for) SOR funding to expand rural SUD workforce through hospital- and ED-based treatments. The SOR grants address the opioid overdose crisis by increasing access to MOUD and support the continuum of care for OUD services.10
Achievements
In the first two years of its funding, the NM Bridge successfully partnered with five hospitals and was written into the state’s 2022-2024 SOR initiative funding to continue their work. These five hospitals include three critical access hospitals, one Indian Health Service hospital, and one acute-care suburban hospital with a large rural catchment area. Several are highly rural–over 100 miles from the nearest tertiary care facility–and serve communities ranging from 20,000 to 70,000 persons. As NM Bridge enters its third year, three more hospitals–two rural referral hospitals and one Indian Health Service facility–have been confirmed.
Pitfalls
Hospitals which initially engaged with NM Bridge but declined to fully pursue the program included one with an already robust MOUD program and two who felt they did not have front-line clinician support. One declined to engage, reporting disagreement that MOUD from the ED is standard of care.
Dr. Greenwood-Ericksen (@MGreenwoodMD) is assistant professor of emergency medicine at the University of New Mexico with a secondary appointment in psychiatry and behavioral sciences department.
Dr. Warrick is a board-certified emergency medicine physician in Albuquerque, New Mexico.
Dr. Ketcham is board certified in both emergency medicine (ABEM) and addiction medicine (ABPM). He serves the New Mexico Bridge Project as the director of clinical implementation, and as an on-call addiction expert for the New Mexico Poison Control Center Opioid Use Disorder Helpline.
Sallyanne Wait is a board-certified nurse practitioner.
Cindy Ketcham has been a registered nurse, practicing in New York, California, and New Mexico since 1989. She is also the director of nursing education for the New Mexico Bridge.
Julie Salvador is an associate professor in the department of psychiatry and behavioral sciences, division of community behavioral health. she serves as the division’s associate director, director of implementation science research, and director of team science.
References
- D’Onofrio G, O’Connor PG, Pantalon MV, et al. Emergency department-initiated buprenorphine/naloxone treatment for opioid dependence: a randomized clinical trial. JAMA. 2015;313(16):1636-1644.
- ACEP. Buprenorphine use in the emergency department tool. ACEP website. https://www.acep.org/patient-care/bupe/. Published 2018. Accessed February 2, 2023.
- Centers for Disease Control. Drug overdose mortality by state. National Center for Health Statistics website. https://www.cdc.gov/nchs/pressroom/sosmap/drug_poisoning_mortality/drug_poisoning.htm. Accessed February 2, 2023.
- Cantor JH, Whaley CM, Stein BD, Powell D. Analysis of substance use disorder treatment admissions in the US by sex and race and ethnicity before and during the COVID-19 pandemic. JAMA Network Open. 2022;5(9):e2232795.
- Altschul DB, Bonham CA, Faulkner MJ, et al. State legislative approach to enumerating behavioral health workforce shortages: lessons learned in New Mexico. Am J Prev Med. 2018;54(6 Suppl 3):S220-S229.
- Larson R. Health care workforce in New Mexico. New Mexico legislative health and human services committee website. https://www.nmlegis.gov/handouts/LHHS%20081721%20Item%206%20UNM%20Workforce%20Annual%20Report%202021.pdf. Published online August 19, 2021. Accessed February 2, 2023.
- Clawar M, Randolph R, Thompson K, Pink GH. Access to care: populations in counties with no FQHC, RHC, or acute care hospital. North Carolina Rural Health Research Program website. https://www.shepscenter.unc.edu/wp-content/uploads/dlm_uploads/2018/01/AccesstoPrimaryCare.pdf. Published January, 2018. Accessed February 2, 2023.
- Beaudoin FL, Jacka BP, Li Y, et al. Effect of a peer-led behavioral intervention for emergency department patients at high risk of fatal opioid overdose: a randomized clinical trial. JAMA Network Open. 2022;5(8):e2225582.
- Qeadan F, Madden EF, Mensah NA, et al. Epidemiological trends in opioid-only and opioid/polysubstance-related death rates among American Indian/Alaska Native populations from 1999 to 2019: a retrospective longitudinal ecological study. BMJ Open. 2022;12(5):e053686.
- U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration. State opioid response grants. https://www.samhsa.gov/grants/grant-announcements/ti-22-005. Published May 19, 2022. Updated September 27, 2022. Accessed February 2, 2023.
Pages: 1 2 3 4 | Multi-Page







No Responses to “The New Mexico Bridge Program”