
It is not uncommon for patients with eye and vision concerns to present initially to the emergency department (ED). Unfortunately, effective, reliable, and easy-to-use tools for eye examination are not readily available to the emergency physicians caring for these patients. Direct ophthalmoscopy, once an integral part of the physical examination, has become a dying art in recent decades.1 Yet, the direct ophthalmoscope is the current standard-of-care tool for emergency physicians to examine the posterior eye, including the retina and the optic nerve. For the best view, dilating drops should be used, but dilation takes time and dilating drops are often not available to emergency physicians. Even with dilation, the pupil offers a small viewing window, hence challenging the clinician to control the ophthalmoscope precisely to get a glimpse of the posterior eye. The examination also requires the clinician to get very close to the patient’s face, and the bright light can cause discomfort to patients who are photosensitive.
Explore This Issue
ACEP Now: Vol 42 – No 03 – March 2023The difficulty of performing the examination and the difficulty of interpreting the findings together limit the real-world utility of this standard-of-care examination technique. Some emergency physicians have adopted newer methods such as fundus photography and ocular ultrasound, but these techniques take time and practice to master. A method of evaluating the posterior eye which could be reliably interpreted by emergency physicians without necessitating extensive prior training would fill an important practice gap.
A pilot study conducted by Song, et al., potentially offers hope to emergency physicians struggling to evaluate the posterior eye, through the use of a robotic eye-imaging device.2 This device was developed by a collaborative team of clinicians and researchers in biomedical engineering, emergency medicine, and ophthalmology at Duke University, and the robotic eye imaging is based on optical coherence tomography (OCT). OCT is an imaging technique widely used in ophthalmology for high-resolution, cross-sectional imaging of the eye. Historically, the use of OCT has been confined to ophthalmology clinics, as manual OCT image acquisition is a fine skill that requires specialized personnel such as ophthalmic photographers. Now with the help of a robot, emergency physicians may also be able to leverage the power of this state-of-the-art imaging technology to diagnose eye diseases.
Image acquisition with the robotic OCT device is as simple as taking a picture with a digital camera: with the press of a button, the robotic OCT device can find the eye autonomously, track any patient and eye movement in real time, and take an image of the posterior eye. Users can visualize cross-sectional views of the retina and optic nerve easily on a computer (Figure 1). Overall, the need for human operation is minimized. In fact, the study reports that the operator was able to control the system remotely (in a separate room from the patient), suggesting the potential for telehealth capabilities in the future. In a busy emergency department, the robotic OCT device could be used to obtain high-quality images of the posterior eye quickly without requiring dedicated, specially trained staff to operate the device. The telehealth capabilities of the device also raise the possibility that these devices could be deployed to rural or outlying EDs where access to both specialized equipment and personnel for ophthalmic examinations are especially limited.
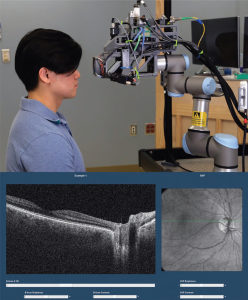
FIGURE 1: Robotic optical coherence tomography (OCT) device (top) and screenshot of OCT viewing software (bottom) showing a cross-sectional OCT image (left) at the level of the green line in the head-on projection (right), which shows the view of fundus examination. (Click to enlarge.)
Importantly, the study suggests that OCT may be of real diagnostic value to emergency physicians. Though most emergency physicians are likely not familiar with the interpretation of OCT images, the nine emergency physicians who participated in the study quickly learned to differentiate abnormal from normal images after a 30-minute training session on the basics of ocular OCT. They were able to interpret the OCT images with 100 percent sensitivity for urgent or emergent abnormalities and 69 percent sensitivity for any posterior eye abnormality when evaluated against reference-standard diagnosis based on a combination of ophthalmology-consultation diagnosis and retina-specialist OCT review. These results were in stark contrast to emergency physician-performed direct ophthalmoscopy, which did not detect any abnormalities in the same patients. As patients with urgent and emergent eye conditions often experience delays in care and subsequent worse outcomes in current clinical practice, these pilot study results indicate that this new technology has the potential to substantially improve the quality of acute eye care by facilitating more accurate ophthalmology referral decisions.
Among the 72 eyes imaged with the robotic OCT device, emergency physicians assessed a broad range of urgent and emergent retinal and optic nerve pathologies such as papilledema, retinal detachment, and retinal vascular occlusion. The three-dimensional nature of OCT imaging makes the detection of these pathologies substantially easier, compared with the two-dimensional view provided by fundus examination. For example, optic disc edema that looks subtle on fundus examination can be obvious on OCT, as elevation of the optic nerve head caused by swelling is readily appreciable in cross sections.3
Currently, the robotic OCT device is still investigational and not commercially available, but this novel technology shows promise in expanding the ability of emergency physicians to diagnose conditions affecting the posterior eye accurately and efficiently.
 Dr. Song is a fourth-year medical student at Duke University. Her research focuses on developing and translating innovative technologies such as robotics and machine learning to improve eye care in non-ophthalmology settings including the emergency department.
Dr. Song is a fourth-year medical student at Duke University. Her research focuses on developing and translating innovative technologies such as robotics and machine learning to improve eye care in non-ophthalmology settings including the emergency department.
 Dr. Kuo is an associate professor of ophthalmology and assistant professor of biomedical engineering at Duke University.
Dr. Kuo is an associate professor of ophthalmology and assistant professor of biomedical engineering at Duke University.
References
- Mackay DD, Garza PS, Bruce BB, Newman NJ, Biousse V. The demise of direct ophthalmoscopy: A modern clinical challenge. Neurol Clin Pract. 2015;5(2):150-157.
- Song A, Roh KM, Lusk JB, et al. Robotic optical coherence tomography retinal imaging for emergency department patients: a pilot study for emergency physicians’ diagnostic performance. Ann Emerg Med. 2023;S0196-0644(22)01196-9.
- Wang JK, Kardon RH, Kupersmith MJ, Garvin MK. Automated quantification of volumetric optic disc swelling in papilledema using spectral-domain optical coherence tomography. Investigative Ophthalmology & Visual Science. 2012;53(7):4069-4075.
Pages: 1 2 3 | Multi-Page




No Responses to “The Real-World Utility of Ophthalmic Tomography”