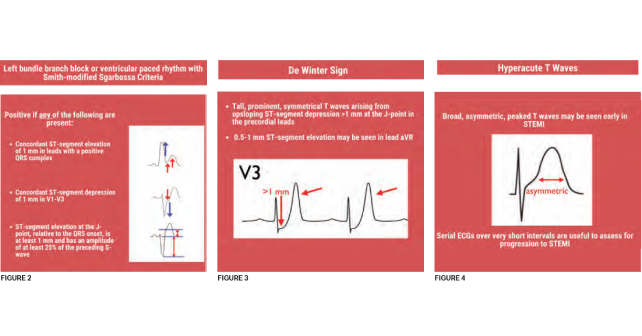
Posterior STEMI (see Figure 1)—Although isolated posterior STEMIs are rare, emergent reperfusion for patients with posterior STEMI is intuitive and hopefully routine practice. Only now, however, is this ECG pattern officially recognized as a STEMI equivalent. No standard ECG leads overlie the posterior wall of the heart, so ischemia in this territory appears as ST-segment depression in leads V1-V4. Criteria include:
- Horizontal ST-segment depression in leads V1-V3, a dominant R wave (R/S ratio >1) in lead V2
- Upright T waves in anterior leads
- A prominent and broad R-wave >30 ms
A posterior ECG with ST-segment elevation in leads V7-V9 may confirm posterior STEMI; however, absence of ≥0.5 mm of elevation in these leads is imperfect and, if an ECG meets other criteria for posterior STEMI, should be treated as such.6
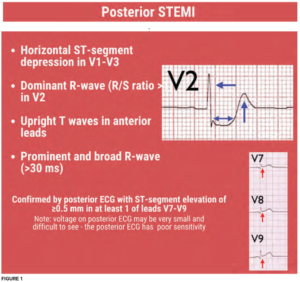
 LBBB or ventricular paced rhythm (VPR) with Sgarbossa or Smith-modified Sgarbossa criteria (see Figure 2)—The presence of an LBBB or VPR distorts the ST segments without necessarily indicating ischemia. Nearly two decades ago, the Sgarbossa criteria were published, allowing clinicians to diagnose ischemia in the presence of LBBB.7,8 Smith et al., further modified the Sgarbossa criteria to improve sensitivity and specificity for occlusion amenable to reperfusion.8,9 The ACC consensus statement states that patients with a LBBB or VPR who have ECG changes meeting Sgarbossa or Smith-modified Sgarbossa criteria should be treated as a “STEMI.”5 Although the consensus statement does not recommend one criterion over the other, the Smith-modified Sgarbossa criteria boasts somewhat better diagnostic ability and may be easier to use since there is no need to score points.9
LBBB or ventricular paced rhythm (VPR) with Sgarbossa or Smith-modified Sgarbossa criteria (see Figure 2)—The presence of an LBBB or VPR distorts the ST segments without necessarily indicating ischemia. Nearly two decades ago, the Sgarbossa criteria were published, allowing clinicians to diagnose ischemia in the presence of LBBB.7,8 Smith et al., further modified the Sgarbossa criteria to improve sensitivity and specificity for occlusion amenable to reperfusion.8,9 The ACC consensus statement states that patients with a LBBB or VPR who have ECG changes meeting Sgarbossa or Smith-modified Sgarbossa criteria should be treated as a “STEMI.”5 Although the consensus statement does not recommend one criterion over the other, the Smith-modified Sgarbossa criteria boasts somewhat better diagnostic ability and may be easier to use since there is no need to score points.9
 de Winter Sign (see Figure 3)—Although described in two percent of cases of anterior myocardial infarction, the tall, symmetrical T waves in precordial leads arising from upsloping ST-segment depression, bearing the eponym of de Winter’s sign, were only described 14 years ago.11 This pattern is indicative of proximal left anterior descending
de Winter Sign (see Figure 3)—Although described in two percent of cases of anterior myocardial infarction, the tall, symmetrical T waves in precordial leads arising from upsloping ST-segment depression, bearing the eponym of de Winter’s sign, were only described 14 years ago.11 This pattern is indicative of proximal left anterior descending
artery occlusion.
- Tall, prominent, symmetrical T waves arising from upsloping ST-segment depression >1 mm at the J-point in the precordial leads
- Slight (0.5-1 mm) ST-segment elevation may be seen in lead aVR
Hyperacute T waves (see Figure 4)—For the past five years, the European Society of Cardiology guidelines has recommended patients with hyperacute T waves and a clinical suspicion of myocardial ischemia receive emergent reperfusion therapy.10 
Hyperacute T waves often represent early signs of occlusion, preceding ST elevation. Specifically, hyperacute T waves are large, relative to the QRS, have a wide base with a rounded peak, and can be associated with other signs of ischemia. These T waves can be tricky to identify as there are several causes of peaked T waves, and are the likeliest of the new STEMI equivalents to cause the most anxiety for emergency clinicians.
Pages: 1 2 3 4 | Single Page




One Response to “The Reperfusion Guidelines Finally Catch Up”
December 21, 2022
Scott R CentersFantastic synopsis and education around STEMI equivalents. I was preparing an educational update for my team when this popped up in my inbox. Dr. Westafer did a much better and more thorough job than I could have.
Kudos and thanks,
Scott R. Centers, MD
Medical Director, Emergency Services
Caromont Health
Gastonia, NC