“Time is myocardium.” Emergency, prehospital, and regional systems have been built around this slogan and are designed to get patients with acute myocardial infarctions, specifically ST-elevation myocardial infarctions (STEMIs), early reperfusion therapy. The American College of Cardiology (ACC) has now caught up with the addition of four “STEMI equivalents,” meaning many more patients should receive cardiac catherization or other means of reperfusion based on more subtle electrocardiogram (ECG) changes.
Explore This Issue
ACEP Now: Vol 41 – No 12 – December 2022How did we get here?
The 2013 American Heart Association (AHA) 2013 guidelines defined STEMI in a rudimentary fashion. Patients with the clinical syndrome fitting with acute coronary syndrome (ACS) must also have at least one of the following (in the absence of left ventricular hypertrophy or left bundle-branch block [LBBB]) on ECG:
- New ST elevation at the J point in at least 2 contiguous leads of ≥2 mm in men or ≥1.5 mm in women in leads V2–V3
- ≥1 mm (0.1 mV) in other contiguous chest leads or the limb leads1
At that time, the guidelines referred to proposed criteria for recognizing ischemia in the presence of an LBBB but did not endorse the Sgarbossa criteria.
Some have argued for years, however, that the STEMI versus non-STEMI dichotomy should be abandoned in favor of targeting occlusion myocardial infarctions (OMIs) for reperfusion therapy, some of which may not meet the ECG definition of STEMI.2,3,4 The most recent consensus statement from the ACC nudges towards recognizing OMI by recommending that four “STEMI equivalents” be treated according to routine STEMI protocols. In fact, the statement highlights the importance of this shift by stating, “the application of STEMI ECG criteria on a standard 12-lead ECG alone will miss a significant minority of patients who have acute coronary occlusion.”5 While the guidelines don’t replace “STEMI” with an inclusive term for those who would benefit from emergent reperfusion therapy, they take a step towards emphasizing that time is myocardium by including ECG patterns indicating early coronary occlusion.
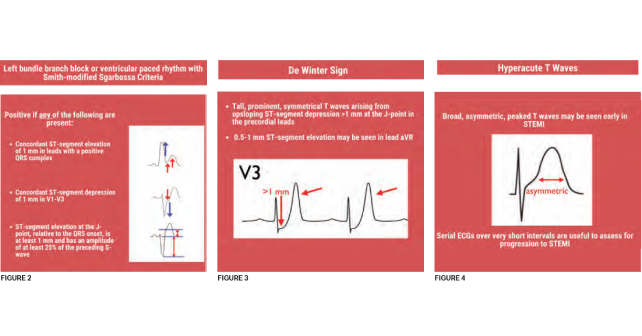
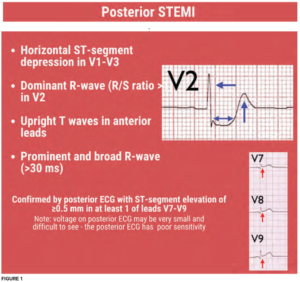
Activate the cath lab or reperfusion treatment for these four ECG patterns
Patients who should be managed as a STEMI and receive early reperfusion therapy are those with traditional STEMI as well as those with one of the following STEMI equivalents: posterior STEMI, LBBB with Sgarbossa or Smith-modified Sgarbossa criteria, DeWinter sign, or hyperacute T waves. The first two STEMI equivalents are unsurprising and have probably triggered cardiac catheterization lab activations across the United States for years. However, the latter STEMI equivalents have only more recently gained recognition.
Posterior STEMI (see Figure 1)—Although isolated posterior STEMIs are rare, emergent reperfusion for patients with posterior STEMI is intuitive and hopefully routine practice. Only now, however, is this ECG pattern officially recognized as a STEMI equivalent. No standard ECG leads overlie the posterior wall of the heart, so ischemia in this territory appears as ST-segment depression in leads V1-V4. Criteria include:
- Horizontal ST-segment depression in leads V1-V3, a dominant R wave (R/S ratio >1) in lead V2
- Upright T waves in anterior leads
- A prominent and broad R-wave >30 ms
A posterior ECG with ST-segment elevation in leads V7-V9 may confirm posterior STEMI; however, absence of ≥0.5 mm of elevation in these leads is imperfect and, if an ECG meets other criteria for posterior STEMI, should be treated as such.6
 LBBB or ventricular paced rhythm (VPR) with Sgarbossa or Smith-modified Sgarbossa criteria (see Figure 2)—The presence of an LBBB or VPR distorts the ST segments without necessarily indicating ischemia. Nearly two decades ago, the Sgarbossa criteria were published, allowing clinicians to diagnose ischemia in the presence of LBBB.7,8 Smith et al., further modified the Sgarbossa criteria to improve sensitivity and specificity for occlusion amenable to reperfusion.8,9 The ACC consensus statement states that patients with a LBBB or VPR who have ECG changes meeting Sgarbossa or Smith-modified Sgarbossa criteria should be treated as a “STEMI.”5 Although the consensus statement does not recommend one criterion over the other, the Smith-modified Sgarbossa criteria boasts somewhat better diagnostic ability and may be easier to use since there is no need to score points.9
LBBB or ventricular paced rhythm (VPR) with Sgarbossa or Smith-modified Sgarbossa criteria (see Figure 2)—The presence of an LBBB or VPR distorts the ST segments without necessarily indicating ischemia. Nearly two decades ago, the Sgarbossa criteria were published, allowing clinicians to diagnose ischemia in the presence of LBBB.7,8 Smith et al., further modified the Sgarbossa criteria to improve sensitivity and specificity for occlusion amenable to reperfusion.8,9 The ACC consensus statement states that patients with a LBBB or VPR who have ECG changes meeting Sgarbossa or Smith-modified Sgarbossa criteria should be treated as a “STEMI.”5 Although the consensus statement does not recommend one criterion over the other, the Smith-modified Sgarbossa criteria boasts somewhat better diagnostic ability and may be easier to use since there is no need to score points.9
 de Winter Sign (see Figure 3)—Although described in two percent of cases of anterior myocardial infarction, the tall, symmetrical T waves in precordial leads arising from upsloping ST-segment depression, bearing the eponym of de Winter’s sign, were only described 14 years ago.11 This pattern is indicative of proximal left anterior descending
de Winter Sign (see Figure 3)—Although described in two percent of cases of anterior myocardial infarction, the tall, symmetrical T waves in precordial leads arising from upsloping ST-segment depression, bearing the eponym of de Winter’s sign, were only described 14 years ago.11 This pattern is indicative of proximal left anterior descending
artery occlusion.
- Tall, prominent, symmetrical T waves arising from upsloping ST-segment depression >1 mm at the J-point in the precordial leads
- Slight (0.5-1 mm) ST-segment elevation may be seen in lead aVR
Hyperacute T waves (see Figure 4)—For the past five years, the European Society of Cardiology guidelines has recommended patients with hyperacute T waves and a clinical suspicion of myocardial ischemia receive emergent reperfusion therapy.10 
Hyperacute T waves often represent early signs of occlusion, preceding ST elevation. Specifically, hyperacute T waves are large, relative to the QRS, have a wide base with a rounded peak, and can be associated with other signs of ischemia. These T waves can be tricky to identify as there are several causes of peaked T waves, and are the likeliest of the new STEMI equivalents to cause the most anxiety for emergency clinicians.
- Broad, asymmetric, peaked T waves may be seen early in STEMI and often evolve into STEMI on serial ECGs
Which ischemic findings don’t make the cut?
Several other ECG findings of acute and subacute ischemia exist. The ACC consensus statement recognizes that ischemia may appear in other forms on ECGs, including Wellen’s syndrome, ischemic T wave inversion or ST-segment depression, and ST-segment elevation in lead aVR with multilead ST-depression. In a minority of these cases, OMI may be present.5 At this time, they recommend that patients with these ischemic ECG patterns be managed according to the 2014 AHA guidelines for the management of non-ST segment ACS.12 In other cases where the ECG may have ischemic findings not meeting previously named criteria, the document recommends serial ECGs, emergent echocardiogram, and/or emergent cardiology consultation.
What now?
Unfortunately, critical changes in guidelines often lack robust implementation plans to ensure that the frontline clinician can quickly integrate the guidelines into practice. Although the ACC consensus statement unequivocally recommends that patients with one of these four STEMI equivalents be treated as a STEMI, institutional and systemic barriers exist. As prehospital systems, hospital systems, and catherization lab teams work to respond to these new criteria, it is critical that emergency physicians integrate these criteria into clinical practice immediately because, after all, time is myocardium.
 Dr. Westafer (@LWestafer) is assistant professor of emergency medicine and emergency medicine research fellowship director at the University of Massachusetts Medical School–Baystate and co-host of FOAMcast.
Dr. Westafer (@LWestafer) is assistant professor of emergency medicine and emergency medicine research fellowship director at the University of Massachusetts Medical School–Baystate and co-host of FOAMcast.
References
- Null N, O’Gara PT, Kushner FG, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction. Circulation. 2013;127(4):e362-e425.
- Aslanger EK, Meyers HP, Smith SW. Time for a new paradigm shift in myocardial infarction. Anatol J Cardiol. 2021;25(3):156-162.
- Meyers HP, Smith SW. Prospective, real-world evidence showing the gap between ST elevation myocardial infarction (STEMI) and occlusion MI (OMI). Int J Cardiol. 2019;293:48-49.
- Meyers P, Weingart S, Smith S. The OMI Manifesto. Blog Post. http://hqmeded-ecg.blogspot.com/2018/04/the-omi-manifesto.html. Published April 1, 2018. Accessed November 13, 2022
- Writing Committee, Kontos MC, de Lemos JA, et al. 2022 ACC expert consensus decision pathway on the evaluation and disposition of acute chest pain in the emergency department: A report of the American College of Cardiology solution set oversight committee. J Am Coll Cardiol. 2022;80:1925-1960. doi:10.1016/j.jacc.2022.08.750
- Wung SF, Drew BJ. New electrocardiographic criteria for posterior wall acute myocardial ischemia validated by a percutaneous transluminal coronary angioplasty model of acute myocardial infarction. Am J Cardiol. 2001;87(8):970-974; A4.
- Sgarbossa EB, Pinski SL, Barbagelata A, et al. Electrocardiographic diagnosis of evolving acute myocardial infarction in the presence of left bundle-branch block. GUSTO-1 (global utilization of streptokinase and tissue plasminogen activator for occluded coronary arteries) investigators. N Engl J Med. 1996;334(8):481-487.
- Smith SW, Dodd KW, Henry TD, Dvorak DM, Pearce LA. Diagnosis of ST-elevation myocardial infarction in the presence of left bundle branch block with the ST-elevation to S-wave ratio in a modified Sgarbossa rule. Ann Emerg Med. 2012;60(6):766-776.
- Meyers HP, Limkakeng AT Jr, Jaffa EJ, et al. Validation of the modified Sgarbossa criteria for acute coronary occlusion in the setting of left bundle branch block: A retrospective case-control study. Am Heart J. 2015;170(6):1255-1264.
- Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119-177.
- de Winter RJ, Verouden NJW, Wellens HJJ, Wilde AAM, Interventional Cardiology Group of the Academic Medical Center. A new ECG sign of proximal LAD occlusion. N Engl J Med. 2008;359(19):2071-2073.
- Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation. 2014;130(25):e344-e426.
Pages: 1 2 3 4 | Multi-Page




One Response to “The Reperfusion Guidelines Finally Catch Up”
December 21, 2022
Scott R CentersFantastic synopsis and education around STEMI equivalents. I was preparing an educational update for my team when this popped up in my inbox. Dr. Westafer did a much better and more thorough job than I could have.
Kudos and thanks,
Scott R. Centers, MD
Medical Director, Emergency Services
Caromont Health
Gastonia, NC