For nearly two years, ACEP has been fighting to ensure that the federal government’s implementation of the No Surprises Act has been in accordance with Congressional intent. Using every channel available on the federal, state, regulatory and legal channels, we have pushed for comprehensive policy and the fair implementation of those policies. Despite our gains on the policy side, the implementation of the law continues to be problematic.
Explore This Issue
ACEP Now: Vol 42 – No 06 – June 2023We’re pushing to fix the flawed implementation on several fronts. From a legal perspective, we have asked the courts to stop the unlawful requirement by the Departments of Health and Human Services, Labor, and Treasury (the Departments) that forces arbiters during the federal independent dispute resolution (IDR) process to illegally emphasize the qualifying payment amount (the QPA, or the median contracted amount) over other factors listed in the statute (patient acuity and complexity; training and experience of the provider; market share of provider/health plan; teaching status and case mix of facility; and previous experience attempting to enter into contractual agreements).
On the regulatory front, our team is pressing HHS to implement and enforce the policy the way it was written. We’re also pressing CMS to: 1) address its excessive increase of the IDR fees; 2) modify the flawed policy that allows limited batching of claims; 3) require more transparency around the calculation of the QPA; and 4) improve its enforcement over health plans that are skirting numerous requirements—most notably not providing the required information that identifies whether a claim is subject to the federal IDR process and not paying physicians what they owe after an arbitration in which the physicians win.
Finally, on the legislative side, we are working with our Congressional allies to put pressure on the Administration to address these significant implementation issues.
Much has happened since the No Surprises Act moved into the implementation phase, so let’s walk through the timeline of key events.
December 2021
ACEP, along with the American Society of Anesthesiologists and the American College of Radiology, filed a lawsuit against the government in Illinois in December 2021, arguing that the second Interim Final Regulation (Final Reg) implementing the No Surprises Act was fatally flawed and should be vacated. The Interim Final Reg set the QPA as the presumptive payment amount for out-of-network services during the IDR process. The Texas Medical Association (TMA) and other plaintiffs filed a similar suit in the Eastern District of Texas, and in early 2022, the court ruled in favor of those plaintiffs, vacating the Interim Final Reg nationwide. ACEP then withdrew its lawsuit and joined other societies in filing amicus briefs in support of the TMA case.
August 2022
When the Departments published the Final Reg, they retracted the rebuttable presumption in favor of the QPA but replaced the presumption with provisions that still tilted the arbitration process in its favor. The TMA again filed suit (TMA II), and again ACEP made the decision to support the TMA case by filing an amicus brief supporting its claims.
January 2023
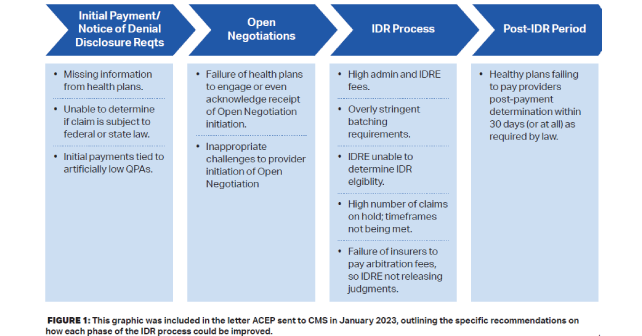
ACEP sent a letter to CMS outlining our concerns with the implementation of the No Surprises Act. We provided specific recommendations on how each phase of the dispute resolution process can be improved. We pointed out that there are issues at every step along the way, from the time physicians receive the initial payment or notice of denial for an out-of-network service, to the Open Negotiations and IDR processes, and ultimately to the post-IDR period.
February 2023
In a big win for ACEP and all emergency physicians, the same federal judge in Texas who ruled in the first TMA lawsuit, Judge Jeremy Kernodle, ruled in favor of the TMA again. The Court’s ruling vacated the sections of the August 2022 Final Reg that require the independent arbiters to consider the QPA first in the IDR process and only to consider other factors in so much as they believe those factors are not already represented in the QPA. Again, the ruling applies to the entire federal IDR process nationwide.
In its opinion, the Court mentioned ACEP’s amicus brief, along with briefs filed by other medical societies. Among other important points regarding the illegality of the Reg’s application, ACEP’s brief emphasized that our members would suffer financial harm because the Reg creates an arbitration process that systematically reduces payments to out-of-network physicians. Judge Kernodle’s opinion stated that “the Final Rule nevertheless continues to place a thumb on the scale for the QPA by requiring arbitrators to begin with the QPA and then imposing restrictions on the non-QPA factors that appear nowhere in the statute.”
Judge Kernodle then rejected the Government’s request that the decision be limited to only the Plaintiffs in the case, holding that vacatur is not unduly disruptive and that the decision must be enforced globally. Arbitrators will continue to decide disputes using all statutory factors as clearly set forth in the Act. He stated, “And here, vacatur would preserve the status quo because arbitrators have been—and are presently—deciding payment disputes pursuant to the statute since the Court vacated the interim final rule nearly a year ago.”
March 2023
In another important advocacy win, CMS issued revised guidance for the independent dispute resolution (IDR) process that took into account the Texas Medical Association court order. The new guidance removed the flawed “double counting” provision and states that independent arbiters must consider all evidence presented to them by the disputing parties (without weighting the qualifying payment amount more heavily than any other factor or assuming that other factors are already incorporated into the qualifying payment amount).
The guidance finally seems to closely reflect what the No Surprises Act statute actually says. We celebrated this as an important advancement in ACEP’s advocacy push to make the arbitration process more fair and balanced.
Also in March, ACEP’s federal advocacy team worked with members of Congress to ensure that HHS Secretary Xavier Becerra would be asked to answer key questions about the implementation of the IDR process during his testimony before several congressional committees regarding President Biden’s fiscal year (FY) 2024 budget.
April 2023
On April 22, the Department of Health and Human Services filed to appeal the ruling to the U.S. Court of Appeals for the Fifth Circuit. If they win their appeal, it could change the guidance that was released in March. For now, that guidance still stands, even though the administration is not enforcing it. Hearings were held for TMA III, which questions the methodology used to calculate the QPA, and TMA IV that argues against the significant increase in the administration fee from $50 to $350 in 2023. ACEP submitted amicus briefs for both earlier this year.
What’s Next?
Our fight continues. We are monitoring the legal situation closely and working with legislators to ensure Congress holds the Administration accountable and implements the carefully crafted statute to the letter of the law.
Leslie Moore is ACEP General Council.
Pages: 1 2 3 | Multi-Page





No Responses to “The Surprise Billing Fight Continues”