Explore This Issue
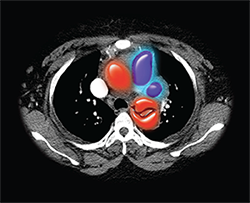
ACEP Now: Vol 34 – No 05 – May 2015Color-enhanced computerized axial tomography (CT) image of a human chest, showing a dissection of the descending thoracic aorta (red fish-mouth shaped structure) in which the wall of the artery tears and blood accumulates within the artery wall.
Image Credit: Living Art Enterprises, LLC / Science Source
In October 2014, the ACEP Board of Directors approved a new clinical policy, developed by ACEP’s Clinical Policies Committee, on the evaluation and management of adult patients with suspected acute nontraumatic thoracic aortic dissection. As is the case with all of ACEP’s clinical policies, it has been published in Annals of Emergency Medicine.1
Acute nontraumatic thoracic aortic dissection is a deadly disease and a can’t-miss diagnosis in the emergency department. Although inpatient mortality from this condition approaches 27 percent, the disease has a very low incidence, and there is little high-quality evidence to guide an approach to diagnosis and management. Considerable medical-legal risk also surrounds its misdiagnosis.
Committee members focused on five critical questions associated with the ED evaluation and management of this condition. A systematic review of the evidence was conducted, and the committee then elucidated a strength of recommendation (A, B, or C) associated with answers to each of the questions (see Table 1). Input was received from ACEP members and individual members of the American Heart Association and the Society for Vascular Surgery during the 60-day open-comment period.
Critical Question 1
In adult patients with suspected acute nontraumatic thoracic aortic dissection, are there clinical decision rules that identify a group of patients at very low risk for the diagnosis of thoracic aortic dissection?
Approximately 8–10 percent of all patients present to the ED with chest pain, and because chest pain is a common complaint in aortic dissection, the treating clinician often considers the diagnosis in patients with this complaint. Therefore, it would be ideal if a clinical decision rule could be used to identify patients at very low risk for having an aortic dissection who do not need to be evaluated for dissection by diagnostic testing. Unfortunately, no such clinical decision rule has been validated in a prospective trial, thus use of clinical decision rules to identify patients at very low risk for acute nontraumatic thoracic aortic dissection was given a Level C recommendation.
Critical Question 2
In adult patients with suspected acute nontraumatic thoracic aortic dissection, is a negative serum D-dimer sufficient to identify a group of patients at very low risk for the diagnosis of thoracic aortic dissection?
Once a clinician decides to evaluate a patient for thoracic aortic dissection, imaging and diagnostic tests must be selected. In recent years, there has been a great deal of literature published on the use of D-dimer in the evaluation of aortic dissection. However, the low quality of these studies resulted in a Level C recommendation for the use of D-dimer to rule out dissection.
Critical Question 3
In adult patients with suspected acute nontraumatic thoracic aortic dissection, is the diagnostic accuracy of a computed tomography angiogram (CTA) at least equivalent to that of transesophageal echocardiogram (TEE) or magnetic resonance angiogram (MRA) to exclude the diagnosis of thoracic aortic dissection?
In the ED, CTA is often used to evaluate patients for suspected thoracic aortic dissection. The Class I, II, and III studies identified in the systematic review of the diagnostic accuracy of CTA reported sensitivities ranging from 93 percent to 100 percent. The evidence demonstrated that the sensitivity of CTA is very similar to that of TEE and MRA, diagnostic modalities that have been suggested as useful for the evaluation of an aortic dissection. CTA is often more readily available in the ED than TEE and MRA, which makes it a practical diagnostic tool. As such, its use received a Level B recommendation.
Critical Question 4
In adult patients with suspected acute nontraumatic thoracic aortic dissection, does an abnormal bedside transthoracic echocardiogram establish the diagnosis of thoracic aortic dissection?
A bedside ultrasound exam such as a transthoracic echocardiogram (TTE) to rule out acute nontraumatic thoracic aortic dissection would be very useful and is becoming a tool in the ED physicians’ diagnostic algorithm as our skills in ultrasound have evolved. However, there are no current studies evaluating ED physician–performed TTE in ruling out thoracic aortic dissection.
The Level B recommendation was, in adult patients with suspected nontraumatic thoracic aortic dissection, do not rely on an abnormal bedside TTE result to definitively establish the diagnosis of thoracic aortic dissection. The Level C (consensus) recommendation was, in adult patients with suspected nontraumatic thoracic aortic dissection, immediate surgical consultation or transfer to a higher level of care should be considered if a TTE is suggestive of aortic dissection.
Critical Question 5
In adult patients with acute nontraumatic thoracic aortic dissection, does targeted heart rate and blood pressure lowering reduce morbidity or mortality?
Once a diagnosis is made, treatment is initiated with the aim of reducing heart rate and blood pressure. Existing guidelines generally recommend aiming for targets of 60 beats/minute and systolic blood pressure below 120 mm Hg. However, there are currently no prospective human trials that demonstrate the superiority of a strategy of decreasing heart rate prior to reducing blood pressure. There is insufficient evidence to definitively identify an optimal target in all patients regardless of age and comorbidities. The Level C recommendation is, in adult patients with acute nontraumatic thoracic aortic dissection, decrease blood pressure and pulse if elevated. However, there are no specific targets that have demonstrated a reduction in morbidity and mortality.
The diagnosis and management of acute thoracic aortic dissection in the ED are challenging. For many reasons, this disease is very difficult to study in randomized controlled trials that might elucidate clearer diagnostic or management pathways. This clinical policy reflects the quality of the literature on this topic and therefore the lack of Level A recommendations that can be made on the management of these patients.
Editor’s Note: The print version of this article omitted the recommendations for critical questions 4 and 5. This version has been updated to include those recommendations.
 Dr. Fredericks is an emergency medicine resident physician at the University of Texas Southwestern in Dallas.
Dr. Fredericks is an emergency medicine resident physician at the University of Texas Southwestern in Dallas.
 Dr. Diercks is professor of emergency medicine and chair of the department of emergency medicine at the University of Texas Southwestern.
Dr. Diercks is professor of emergency medicine and chair of the department of emergency medicine at the University of Texas Southwestern.
Reference
Pages: 1 2 3 | Multi-Page





No Responses to “Thoracic Aortic Dissection Clinical Policy Approved by ACEP Board”