Explore This Issue
ACEP Now: Vol 36 – No 03 – March 2017(click for larger image)
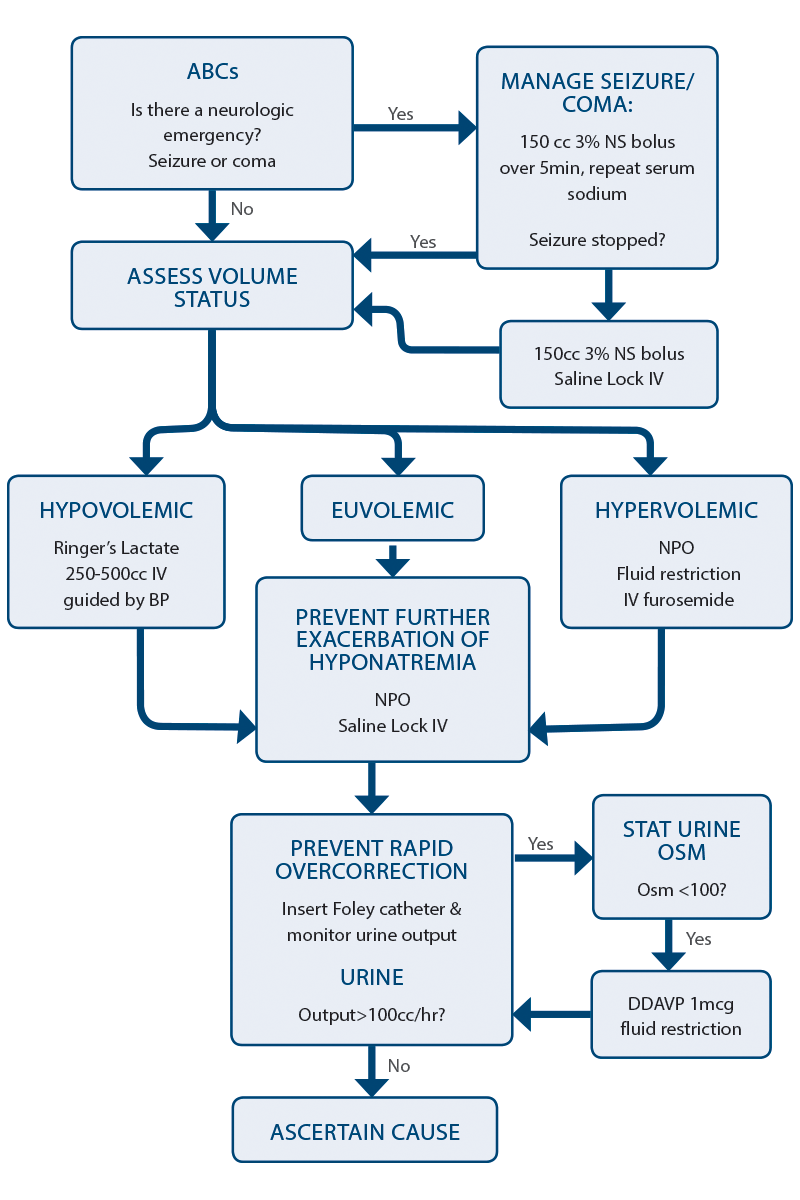
Figure 1: Algorithm for Managing Hyponatremia in the Emergency Department

Hyponatremia is the most common electrolyte abnormality seen in clinical practice. Not only is it found in about 20 percent of hospital admissions, but hyponatremia is an independent predictor of mortality. Part of the reason for this is, unfortunately, iatrogenic because misguided efforts to correct hyponatremia can be devastating for the patient and are a common reason for medical-legal action. Overcorrection can put patients at risk for osmotic demyelination syndrome (ODS), formerly known as central pontine myelinolysis.
There are two factors that influence how symptomatic a patient will be from hyponatremia: severity of hyponatremia and the acuity of onset. The lower the sodium and the faster the fall, the more symptomatic a patient will become. The rapidity of onset is important to ascertain because aggressive rapid correction of a slow-onset hyponatremia is more likely to result in complications. Symptoms are often vague and nonspecific and include headache, irritability, lethargy, confusion, agitation, and unstable gait leading to a fall. Thus, hyponatremia is often discovered incidentally on “routine” blood work.
Step-Wise Approach to Managing Hyponatremia
1. Treat neurologic emergencies related to hyponatremia. In the event of a seizure, coma, or suspected cerebral herniation as a result of hyponatremia, 3% hypertonic saline 150 mL IV over five to 10 minutes should be administered as soon as possible. If the patient does not improve clinically after the first bolus, repeat a second bolus of hypertonic saline. It is important to stop all fluids after the second bolus to avoid raising the serum sodium any further. If hypertonic saline is not readily available, administer one ampule of sodium bicarbonate over five minutes.
2. Defend the intravascular volume. In order to maintain a normal intravascular volume, the patient’s volume status must first be estimated. Although volume status is difficult to assess with any accuracy at the bedside, a clinical assessment with attention to the patient’s history, heart rate, blood pressure, jugular venous pressure, the presence of pedal and sacral edema, the presence of a postural drop, and point-of-care ultrasound is usually adequate to make a rough estimation of whether the patient is significantly hypovolemic (requiring fluid resuscitation) or significantly hypervolemic (requiring fluid restriction or diuretics).
In a patient who is hypovolemic and hyponatremic, the priority is to restore adequate circulating volume. This takes priority over any concerns that the hyponatremia might be corrected too rapidly and lead to ODS.
Which type of fluid is best? Ringer’s lactate has a sodium concentration of 128 mmol/L, which is more isotonic to the hyponatremic patient. Administering Ringer’s lactate will likely result in a slower rise in serum sodium than normal saline and therefore have a lower risk of causing ODS. I therefore recommend Ringer’s lactate as the fluid of choice for resuscitation of the hypovolemic/hyponatremic patient.
For hyponatremic patients deemed to be hypervolemic, management includes sodium restriction, free water restriction, and diuretics.
Euvolemic patients with hyponatremia do not require any particular treatment to defend intravascular volume, and management should concentrate on preventing worsening hyponatremia. The syndrome of inappropriate antidiuretic hormone (ADH) secretion (SIADH) is hyponatremia and hypo-osmolality secondary to secretion of ADH despite normal or increased plasma volume. This results in impaired water excretion. It is important to understand that SIADH is a result of an excess of water rather than a deficiency of sodium. SIADH is usually caused by a medication, cancer, respiratory illness, or central nervous system illness.
3. Prevent worsening hyponatremia. After restoring adequate circulating volume, the goal is to prevent further exacerbation of the hyponatremia by strict fluid restriction and an IV saline lock. It is vital to communicate this to the patient’s family and health care team. Water can literally kill the patient!
4. Prevent rapid overcorrection: the rule of 100s. It is important to understand that the fluid itself that is given to the hyponatremic patient is not the cause of a rapid increase in the serum sodium but rather the free water diuresis that results shortly afterwards. Thus, monitoring the urine output is key in preventing overcorrection and possible complications. To prevent rapid overcorrection:
- Insert a urinary catheter and monitor ins and outs.
- If urine output >100 cc/hour, send a STAT urine osmolarity and sodium.
- If urine osmolarity <100, consider 1 mg desmopressin (DDAVP) IV.
- Continue following steps 2–4 as per urine output.
Correcting Hyponatremia: the Rule of 6s
“Six in six hours for severe symptoms, then stop. Six a day makes sense for safety.”
If you need to rapidly increase serum sodium due to a neurological emergency, do not correct more than 6 mmol. Do not exceed an increase of sodium of more than 6 mmol/day. While different sources will cite different ranges, targeting six is a conservative approach.
Ascertain the Cause of Hyponatremia
- Assess the chief complaint: Search for conditions that can increase output or decrease intake such as vomiting and diarrhea, pain, or altered level of awareness.
- Review the medication list: Search for those that cause SIADH, especially thiazide diuretics and selective serotonin reuptake inhibitors. Patients who have been on chronic steroids may have adrenal insufficiency as a cause for their hyponatremia.
- Evaluate the past medical history: Look for a history of end organ failure (congestive heart failure, liver failure, or renal failure) or cancers (a common cause of SIADH).
- Evaluate the lab work: Assess the glucose (hyperglycemia), potassium (hyperkalemia may suggest adrenal insufficiency), and thyroid-stimulating hormone (hypothyroidism).
Next time a weak and dizzy older person presents to your emergency department with a serum sodium concentration in the boots, simply follow this algorithm (see Figure 1) so that your patient will make a smooth recovery and you won’t be asked by the admitting physician a week later, “Do you remember that hyponatremic patient you saw the other day?”
Thanks to Dr. Melanie Baimel and Dr. Edward Etchells for their contributions to the EM Cases podcast that inspired this article.
 Dr. Helman is an emergency physician at North York General Hospital in Toronto. He is an assistant professor at the University of Toronto, Division of Emergency Medicine, and the education innovation lead at the Schwartz/Reisman Emergency Medicine Institute. He is the founder and host of Emergency Medicine Cases podcast and website.
Dr. Helman is an emergency physician at North York General Hospital in Toronto. He is an assistant professor at the University of Toronto, Division of Emergency Medicine, and the education innovation lead at the Schwartz/Reisman Emergency Medicine Institute. He is the founder and host of Emergency Medicine Cases podcast and website.
Pages: 1 2 3 | Multi-Page




No Responses to “Tips to Assess Rapid Onset of Hyponatremia to Prevent Overcorrection and Diagnose Underlying Cause”