In the emergency department, isolated fibular ankle fractures are frequently characterized using the Danis-Weber classification system. This fracture classification system, based on the level of the fibular fracture in relation to the ankle joint, can help determine which injuries are likely to require surgical intervention. The Weber classification is simple, reliable, and reproducible, and thus it has been utilized routinely by emergency physicians.1,2
Explore This Issue
ACEP Now: Vol 39 – No 04 – April 2020Injuries to the distal fibula, below the talar dome, are classified as type A and are stable fractures. Weber C fractures are above the ankle joint and are associated with a syndesmotic injury. Weber C fractures are almost always unstable and require surgical intervention. Weber B fractures occur at the level of the tibiofibular ligaments, just above the talar dome, and happen primarily through a mechanism of ankle supination and external rotation (SER).3 These type B fractures are sometimes stable, and patients can ambulate on them as tolerated; in other cases, they are unstable and require open reduction and internal fixation (ORIF). The focus of this article is to help emergency physicians choose the proper method for determining that stability.
Do They Need an Operation?
The primary consideration regarding need for operative management of a closed ankle fracture is stability. In general, most stable ankle fractures can undergo nonoperative management by a primary care physician. Unstable ankle fractures are one of the primary indications for orthopedic referral. Any bi- or trimalleolar fracture should be considered unstable because of the disruption of the bony architecture on both the medial and lateral side of the joint.
With Weber B fractures, the stability of the ankle joint depends on injury to the tibiofibular ligaments and the deltoid ligament. The deltoid ligament, which runs from the medial malleolus to the calcaneus, talus, and navicular bones, plays a vital role in maintaining correct talus positioning. A talar shift of 1 mm results in a 42 percent decrease in tibiotalar contact area, which can lead to significant increases in contact stress.4 In what appears as an otherwise isolated Weber B fibular injury, a tear of the deltoid ligament can be considered “equivalent to a medial malleolar fracture,” qualifying the fracture mechanically as unstable, thus requiring operative management.5
Clinical signs such as medial ankle pain, swelling, and ecchymosis are not reliable in identifying a deltoid ligament injury.3 For this reason, assessing deltoid ligament integrity is of critical importance in determining the stability of an ankle fracture. To do this, emergency physicians need to employ stress radiographs to assess the stability of the ankle joint.
Evaluation
When evaluating a Weber B fracture, if the initial imaging does not demonstrate obvious evidence of tibiotalar instability, ankle stress testing is indicated. There are three primary methods of performing an ankle stress test. These include manual, gravity, and weight-bearing techniques.
Manual stress testing has historically been the method utilized to evaluate the stability of the ankle joint. This method involves keeping the ankle at neutral dorsiflexion, rotating the tibia internally at 10°, and applying 8 to 20 pounds of external rotation at the foot.3 This typically requires a physician going to the radiology suite to perform the stress test.
Gravity stress is typically performed with the patient lying in lateral decubitus with the injured side down, allowing the foot and ankle to create a lateral force across the ankle joint, with the foot resting in natural plantar flexion and the leg internally rotated at 10° to 15° (see Figure 1).6 Gravity stress has been shown to be as reliable and less painful than manual stress testing.6,7
Weight-bearing films are a relatively new method of testing for medial stability. Despite initial cadaveric studies demonstrating that weight-bearing films did not accurately provide radiographic evidence of instability, recent clinical studies have shown that weight-bearing radiographs are predictive of stability and that gravity stress radiographs likely overestimate the instability, resulting in up to a tenfold increase in surgeries when a medial clear space (MCS) cutoff of 4 mm is used.8–11 One recent study compared patients who had a borderline unstable ankle based on gravity stress imaging (MCS 4–7 mm) but stability on the weight-bearing imaging to patients who had a stable ankle based on gravity and weight-bearing imaging. There was no functional outcome difference between the two cohorts of patients who elected to be managed nonoperatively.10 The most compelling argument for weight-bearing films is that they stress the ankle joint under physiological conditions that measure stability under realistic and reproducible conditions.
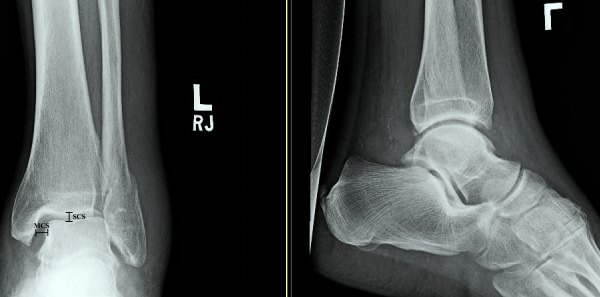
Figure 2: Normal ankle mortise view with demonstrated medial clear space (MCS) and superior clear space (SCS).
Joseph Noack & Spencer Tomberg
Like gravity stress imaging, weight-bearing films can be performed by a radiology technician without physician assistance. The weight-bearing technique is more reproducible and takes less radiology technician training than either gravity stress or manual stress views.10 However, from an emergency medicine perspective, one of the most glaring questions is whether patients with an acutely injured ankle can bear enough weight to get adequate radiographs, as the studies comparing stress techniques have been completed in orthopedic clinics three to 10 days after the initial injury. We could not find data pertaining to this particular question.
MRI can be used to evaluate the deltoid ligament, but the degree of the tear does not always equate to instability on stress radiographs.12
Specific parameters are evaluated in each stress view of the ankle. For gravity stress views, consensus is leaning to a value for the MCS of <7 mm to define a stable ankle joint. An MCS >4 mm is the historical value used to indicate operative management, but this value has been shown to lead to a high false-positive rate and unnecessary surgeries, of which 10 percent have surgical complications.13,14 An MCS greater than the superior clear space (SCS) of 1 mm or more on mortise view is another sign of ankle instability (see Figure 2). Finally, if the injured side has an MCS that is >2 mm wider than the uninjured side, the ankle can be considered unstable. Any of these radiographic abnormalities on initial imaging suggest a clinically significant injury to the deltoid ligament and ankle instability.13 While the trend is toward adopting the 6 mm threshold for MCS, there is no consensus among orthopedic surgeons and your consultant may use stricter guidelines.6,13
Conclusion
Ankle fractures are a common presentation in emergency departments. While some fractures demonstrate either clear stability or instability based on initial radiographs, Weber B fractures require more diagnostic testing to evaluate the stability of the deltoid and tibiofibular ligaments. Historically, this has been done with manual stress views. However, the clear trend is that gravity and weight-bearing stress radiographs are able to detect unstable ankles at the same rate, utilize less physician resources, and are less painful for patients.
 Dr. Noack is a third-year emergency medicine resident at Denver Health Medical Center.
Dr. Noack is a third-year emergency medicine resident at Denver Health Medical Center.
 Dr. Tomberg is an emergency physician at Denver Health Medical Center. He works in the ski clinic at the base of Winter Park Ski Area, the Denver Health Emergency Department, the Denver Health Adult Urgent Care Center, and the sports medicine department at Denver Health.
Dr. Tomberg is an emergency physician at Denver Health Medical Center. He works in the ski clinic at the base of Winter Park Ski Area, the Denver Health Emergency Department, the Denver Health Adult Urgent Care Center, and the sports medicine department at Denver Health.
References
- Fonseca LLD, Nunes IG, Nogueira RR, et al. Reproducibility of the Lauge-Hansen, Danis-Weber, and AO classifications for ankle fractures. Rev Bras Ortop. 2017;53(1):101-106.
- Malek IA, Machani B, Mevcha AM, et al. Inter-observer reliability and intra-observer reproducibility of the Weber classification of ankle fractures. J Bone Joint Surg Br. 2006;88(9):1204-1206.
- van den Bekerom MP, Mutsaerts EL, van Dijk CN. Evaluation of the integrity of the deltoid ligament in supination external rotation ankle fractures: a systematic review of the literature. Arch Orthop Trauma Surg. 2009;129(2):227-235.
- Ramsey PL, Hamilton W. Changes in tibiotalar area of contact caused by lateral talar shift. J Bone Joint Surg Am. 1976;58(3):356-357.
- Yufit P, Seligson D. Malleolar ankle fractures. A guide to evaluation and treatment. Orthop Trauma. 2010;24(4):286-297.
- Aiyer AA, Zachwieja EC, Lawrie CM, et al. Management of isolated lateral malleolus fractures. J Am Acad Orthop Surg. 2019;27(2):50-59.
- Schock HJ, Pinzur M, Manion L, et al. The use of gravity or manual-stress radiographs in the assessment of supination-external rotation fractures of the ankle. J Bone Joint Surg Br. 2007;89(8):1055-1059.
- Stewart C, Saleem O, Mukherjee DP, et al. Axial load weightbearing radiography in determining lateral malleolus fracture stability: a cadaveric study. Foot Ankle Int. 2012;33(7):548-552.
- Holmes JR, Acker WB 2nd, Murphy JM, et al. A novel algorithm for isolated Weber B ankle fractures: a retrospective review of 51 nonsurgically treated patients. J Am Acad Orthop Surg. 2016;24(9):645-652.
- Seidel A, Krause F, Weber M. Weightbearing vs gravity stress radiographs for stability evaluation of supination-external rotation fractures of the ankle. Foot Ankle Int. 2017;38(7):736-744.
- Dawe EJ, Shafafy R, Quayle J, et al. The effect of different methods of stability assessment on fixation rate and complications in supination external rotation (SER) 2/4 ankle fractures. Foot Ankle Surg. 2015;21(2):86-90.
- Nortunen S, Lepojärvi S, Savola O, et al. Stability assessment of the ankle mortise in supination-external rotation-type ankle fractures: lack of additional diagnostic value of MRI. J Bone Joint Surg Am. 2014;96(22):1855-1862.
- van Leeuwen CAT, Hoffman RPC, Donken CCMA, et al. The diagnosis and treatment of isolated type B fibular fractures: results of a nationwide survey. Injury. 2019;50(2):579-589.
- Schuberth JM, Collman DR, Rush SM, et al. Deltoid ligament integrity in lateral malleolar fractures: a comparative analysis of arthroscopic and radiographic assessments. J Foot Ankle Surg. 2004;43(1):20-29.
Pages: 1 2 3 4 | Multi-Page




One Response to “Tips for Managing Weber B Ankle Fractures”
May 19, 2020
Huda NaeemIs there an app for this ACEPNOW?