The Case
A 28-year-old male presents after a motorcycle crash. He has right lower leg pain and tenderness. His pulses and nerve function are intact. An X-ray shows a tibial shaft fracture. After splinting the leg and calling orthopedics, the physician finds the patient is anxious and reporting worsening pain despite IV morphine. His leg has become pale and cool, with absent pulses.
Explore This Issue
ACEP Now: Vol 38 – No 10 – October 2019Clinical Presentation
This textbook presentation of compartment syndrome seems easy. Real cases often are not. In emergency medicine, we deal with critically ill patients who may require sedation and/or intubation, and diagnosing compartment syndrome in patients can require some finesse. Not only can compartment syndrome cause major complications, but frighteningly, 23 percent of medicolegal cases involving compartment syndrome were due to misdiagnosis, while 32 percent of cases were due to delayed treatment.1
Compartment syndrome is due to excessive pressure in a fascial compartment, either through increased volume in a fixed compartment (edema, hematoma) or reduced size of a compartment (tight cast, wound dressings, poor body positioning, etc.).2-4 As pressure builds, lymphatic, capillary, and venous blood flow decrease.5-7 This results in reduced arterial blood flow and tissue ischemia, followed by necrosis, neurological damage, contractures, and, in severe circumstances, need for amputation.8-11 Rhabdomyolysis may also occur with muscle breakdown.8-11 Unfortunately, muscle necrosis can occur quickly; in one study, one-third of cases experienced muscle necrosis within three hours of injury.12
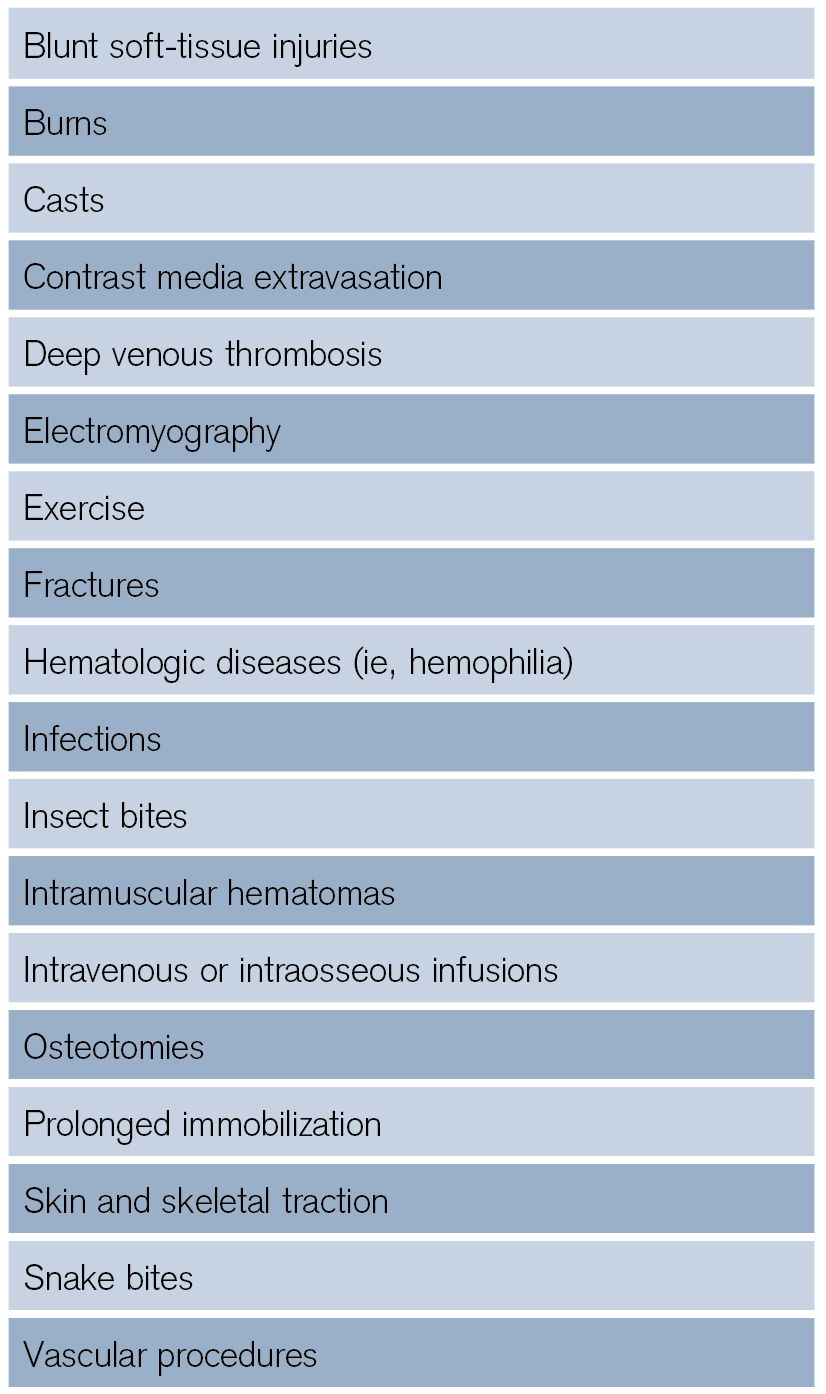
The most commonly affected region is the anterior compartment of the lower leg, and compartment syndrome can occur in up to 10 percent of patients with tibial fracture.5,6,13-15 Male patients age 20 to 40 years are particularly at risk, as this age group has a higher risk of high-energy injuries, greater muscle bulk (more swelling), and stronger fascia. However, the elderly are also at higher risk due to baseline hypertension and reduced compartment perfusion.4 Fractures are the most common etiology. Open fractures can also cause compartment syndrome, as the small fascial/skin breaks do not adequately release pressure.13,16-18 Other causes are shown in Table 1.
How useful are historical features? Unfortunately, early findings can be subtle or not detected in patients with altered mental status, major trauma, substance use, and extremes of age.2-4,18 Classically, the earliest symptom is pain out of proportion to the exam (as with other conditions including necrotizing fasciitis and mesenteric ischemia). Patients typically describe this pain as a deep, severe pain that worsens with passive stretch.3,19-21 While this seems relatively straightforward, data suggest that severe pain has poor sensitivity, as pain is typically subjective.19 If ischemia develops, pain may vanish with necrosis.18 Other late symptoms include sensory changes/paresthesias and focal motor deficits.5,6,19
Diagnosis
Is your bedside exam reliable? While we are taught about the classic findings of pain with passive stretch, a tense/firm compartment, swelling, focal motor/sensory changes, and decreased pulses, these are not always present and have poor sensitivity.3-5,14,19 Digital palpation has a sensitivity under 50 percent for detection of compartment syndrome affecting the hand and under 25 percent for the leg.22,23 Paralysis and absent pulses are rare, and palpating a tense or firm compartment is not reliable. Swelling of the affected area may be present in only half of patients.3,14,19 Table 2 demonstrates the sensitivity and specificity of exam findings.19
As you can see from Table 2, many classic findings are highly specific but poorly sensitive.
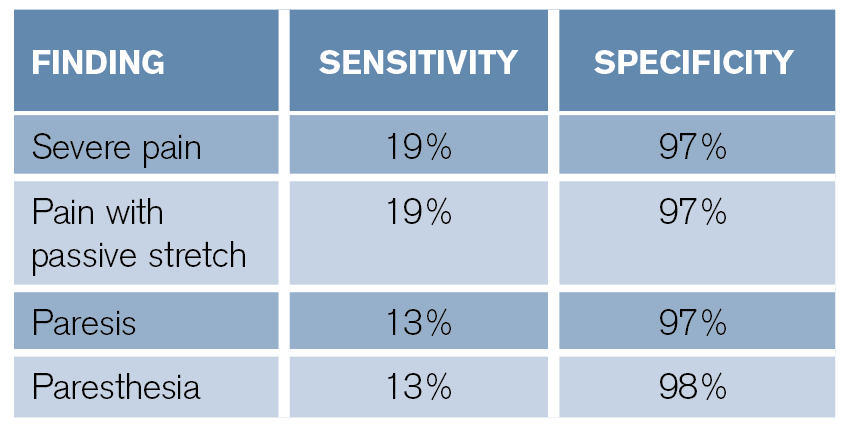
Table 2: Diagnostic Accuracy of Exam Findings19
What happens if you combine signs and symptoms? A combination of pain with passive stretch, pain at rest, and paresthesias has a sensitivity of 93 percent for diagnosis, and the addition of paresis increases sensitivity to 98 percent.19 However, do not rely on the absence of any classic isolated findings. Other items that complicate diagnosis based on history and exam include clinician inexperience, sedation, polytrauma, and intoxication.8,19,24,25
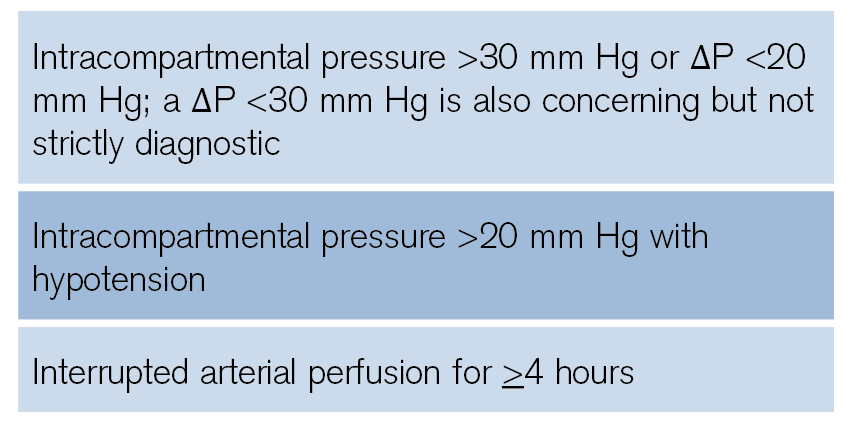
Table 3: Clinical Signs Suggestive of Compartment Syndrome
What about other tools? Abnormal pulse oximetry may indicate compartment syndrome.3,18,19 However, you cannot use this to exclude the condition. Rhabdomyolysis is present in up to 40 percent of patients with compartment syndrome, so be sure to check creatine kinase levels, renal function, and electrolytes.26-28
The most reliable bedside data can be obtained by measuring intracompartmental pressure. Options include a solid-state transducer intracompartmental catheter (STC) device (eg, a Stryker monitor) or other needle manometer/arterial line setups.4-6,19 The Stryker monitor has a diagnostic sensitivity around 95 percent, with specificity greater than 98 percent.29-31 Make sure to place the catheter within 5 cm of the fracture/injury level. However, the catheter tip should be outside the actual site of the fracture. Also ensure the pressure transducer and catheter tip are at the same height.24,32-35

Figure 1: Stryker intracompartmental pressure monitoring device. To measure the pressure in a particular compartment, set the device to zero, insert the needle into the compartment and perpendicular to the skin, inject 0.3 mL sterile saline, and read the pressure displayed on the screen.

Figure 2: Stryker intracompartmental pressure monitoring device being inserted into the lower leg.
After obtaining the intracompartmental pressure, you can use an absolute intracompartmental pressure of 30–40 mm Hg as diagnostic, but using a true intracompartmental pressure alone is problematic, as different compartments have varying pressure thresholds and patients may have varying absolute pressures.5,6,18,36 Some advocate using a perfusion pressure or differential pressure, which is calculated by subtracting the intracompartmental pressure from the diastolic pressure.4-6,19 A differential pressure (ΔP = compartmental pressure – diastolic blood pressure) of <20 mm Hg is diagnostic. While higher intracompartmental pressures can cause severe damage over a short time period, relatively lower but elevated intracompartmental pressures for long time periods can also cause severe tissue damage. Also, an absolute intracompartmental pressure >20 mm Hg in the setting of hypotension should be considered diagnostic.4-6,19,24 If the initial pressure is normal but the clinical picture fits compartment syndrome, a repeat measurement as well as pressure measurements in surrounding compartments are recommended.4-16,24 Table 3 shows situations that are diagnostic of compartment pressure.
Treatment

Figure 3: Lower leg fasciotomy
If you suspect compartment syndrome for any reason, emergently consult orthopedics. Once a motor nerve deficit is present, full recovery is rare.3,4,24 The orthopedic surgeon will most likely want to obtain their own pressure assessment, so the earlier you discuss the case with the surgeon, the better. If orthopedics is unavailable, discuss the case with a surgeon able to complete fasciotomy.
Definitive therapy is fasciotomy. In the emergency department, provide analgesia, resuscitate the patient, remove any constrictive dressings/bandages, reduce fractures, and elevate the affected extremity to heart level.3-5,17,26 Removing an external compressive device such as a tight cast can reduce pressure by up to 85 percent.5,6,38,39
Case Resolution
The patient has a firm lower leg with absent pulses. Passive movement of the foot causes extreme pain. Orthopedic surgery is consulted, and the patient is taken immediately to the operating room.
The views expressed in this publication do not reflect the views or opinions of the U.S. government, Department of Defense, U.S. Army, U.S. Air Force, Brooke Army Medical Center, or SAUSHEC EM Residency Program.
Dr. Long is an emergency physician in the San Antonio Uniformed Services Health Education Consortium at Fort Sam Houston, Texas.
 Dr. Koyfman (@EMHighAK) is assistant professor of emergency medicine at UT Southwestern Medical Center and an attending physician at Parkland Memorial Hospital in Dallas.
Dr. Koyfman (@EMHighAK) is assistant professor of emergency medicine at UT Southwestern Medical Center and an attending physician at Parkland Memorial Hospital in Dallas.
References
- Marchesi M, Marchesi A, Calori GM, et al. A sneaky surgical emergency: acute compartment syndrome. Retrospective analysis of 66 closed claims, medico-legal pitfalls and damages evaluation. Injury. 2014;45(suppl 6):S16-20.
- McQueen MM, Gaston P, Court-Brown CM. Acute compartment syndrome. Who is at risk? J Bone Joint Surg Br. 2000;82(2):200-203.
- Donaldson J, Haddad B, Khan WS. The pathophysiology, diagnosis and current management of acute compartment syndrome. Open Orthop J. 2014;8:185-193.
- Duckworth AD, McQueen MM. The diagnosis of acute compartment syndrome: a critical analysis review. JBJS Rev. 2017;5(12):e1.
- Schmidt AH. Acute compartment syndrome. Orthop Clin North Am. 2016;47(3):517-525.
- Schmidt AH. Acute compartment syndrome. Injury. 2017;48(suppl 1):S22-S25.
- Mabvuure NT, Malahias M, Hindocha S, et al. Acute compartment syndrome of the limbs: current concepts and management. Open Orthop J. 2012;6:535-543.
- Mithöfer K, Lhowe DW, Vrahas MS, et al. Clinical spectrum of acute compartment syndrome of the thigh and its relation to associated injuries. Clin Orthop Relat Res. 2004;425:223-229.
- Finkelstein JA, Hunter GA, Hu RW. Lower limb compartment syndrome: course after delayed fasciotomy. J Trauma. 1996;40(3):342-344.
- Gourgiotis S, Villias C, Germano S, et al. Acute limb compartment syndrome: a review. J Surg Educ. 2007;64(3):178-186.
- Kalyani BS, Fisher BE, Roberts CS, et al. Compartment syndrome of the forearm: a systematic review. J Hand Surg Am. 2011;36(3):535-543.
- Vaillancourt C, Shrier I, Vandal A, et al. Acute compartment syndrome: how long before muscle necrosis occurs? CJEM. 2004;6(3):147-154.
- Mauser N, Gissel H, Henderson C, et al. Acute lower-leg compartment syndrome. Orthopedics. 2013;36(8):619-624.
- Al-Dadah OQ, Darrah C, Cooper A, et al. Continuous compartment pressure monitoring vs. clinical monitoring in tibial diaphyseal fractures. Injury. 2008;39(10):1204-1209.
- McQueen MM, Christie J, Court-Brown CM. Acute compartment syndrome in tibial diaphyseal fractures. J Bone Joint Surg Br. 1996;78(1):95-98.
- McQueen MM, Court-Brown CM. Compartment monitoring in tibial fractures. The pressure threshold for decompression. J Bone Joint Surg Br. 1996;78:99-104.
- Taylor RM, Sullivan MP, Mehta S. Acute compartment syndrome: obtaining diagnosis, providing treatment, and minimizing medicolegal risk. Curr Rev Musculoskelet Med. 2012;5(3):206-213.
- Via AG, Oliva F, Spoliti M, et al. Acute compartment syndrome. Muscles Ligaments Tendons J. 2015;5(1):18-22.
- Ulmer T. The clinical diagnosis of compartment syndrome of the lower leg: are clinical findings predictive of the disorder? J Orthop Trauma. 2002;16:572-577.
- Shadgan B, Pereira G, Menon M, et al. Risk factors for acute compartment syndrome of the leg associated with tibial diaphyseal fractures in adults. J Orthop Traumatol. 2015;16(3):185-192.
- McQueen MM, Duckworth AD, Aitken SA, et al. The estimated sensitivity and specificity of compartment pressure monitoring for acute compartment syndrome. J Bone Joint Surg Am. 2013;95(8):673-677.
- Wong JC, Vosbikian MM, Dwyer JM, et al. Accuracy of measurement of hand compartment pressures: a cadaveric study. J Hand Surg Am. 2015;40(4):701-706.
- Shuler FD, Dietz MJ. Physicians’ ability to manually detect isolated elevations in leg intracompartmental pressure. J Bone Joint Surg Am. 2010;92(2):361-367.
- McQueen MM. Acute compartment syndrome. In: Bucholz RW, Court-Brown CM, Heckman JD, Tornetta P III, eds. Rockwood and Green’s Fractures in Adults. 7th ed. Philadelphia: Lippincott Williams & Wilkins; 2010:689-708.
- Roberts CS, Gorczyca JT, Ring D, et al. Diagnosis and treatment of less common compartment syndromes of the upper and lower extremities: current evidence and best practices. Instr Course Lect. 2011;60:43-50.
- Raza H, Mahapatra A. Acute compartment syndrome in orthopedics: causes, diagnosis, and management. Adv Orthop. 2015;2015:543412.
- Tsai WH, Hunag ST, Liu WC. High risk of rhabdomyolysis and acute kidney injury after traumatic limb compartment syndrome. Ann Plast Surg. 2015;74(suppl 2):S158–S161.
- Lima RS, da Silva Junior GB, Liborio AB, et al. Acute kidney injury due to rhabdomyolysis. Saudi J Kidney Dis Transpl. 2008;19(5):721-729.
- McQueen MM, Duckworth AD, Aitken SA, et al. The estimated sensitivity and specificity of compartment pressure monitoring for acute compartment syndrome. J Bone Joint Surg Am. 2013;95(8):673-677.
- Large TM, Agel J, Holtzman DJ, et al. Interobserver variability in the measurement of lower leg compartment pressures. J Orthop Trauma. 2015;29(7):316-321.
- Boody AR, Wongworawat MD. Accuracy in the measurement of compartment pressures: a comparison of three commonly used devices. J Bone Joint Surg Am. 2005;87(11):2415-2422.
- Heckman MM, Whitesides TE Jr, Grewe SR, et al. Compartment pressure in association with closed tibial fractures. The relationship between tissue pressure, compartment, and the distance from the site of the fracture. J Bone Joint Surg Am. 1994;76(9):1285-1292.
- Matava MJ, Whitesides TE Jr, Seiler JG 3rd, et al. Determination of the compartment pressure threshold of muscle ischemia in a canine model. J Trauma. 1994;37(1):50-58.
- Saikia KC, Bhattacharya TD, Agarwala V. Anterior compartment pressure measurement in closed fractures of leg. Indian J Orthop. 2008;42(2):217-221.
- Harris IA, Kadir A, Donald G. Continuous compartment pressure monitoring for tibia fractures: does it influence outcome? J Trauma. 2006;60(6):1330-1335; discussion 1335.
- Mubarak SJ, Owen CA, Hargens AR, et al. Acute compartment syndromes: diagnosis and treatment with the aid of the wick catheter. J Bone Joint Surg Am. 1978;60(8):1091-1095.
- Sheridan GW, Matsen FA 3rd. Fasciotomy in the treatment of the acute compartment syndrome. J Bone Joint Surg Am. 1976;58(1):112-115.
- Mars M, Hadley GP. Raised compartmental pressure in children: a basis for management. Injury. 1998;29(3):183-185.
- Hoover TJ, Siefert JA. Soft tissue complications of orthopedic emergencies. Emerg Med Clin North Am. 2000;18(1):115-139.
Pages: 1 2 3 4 | Multi-Page



3 Responses to “Tips for Quickly Diagnosing Compartment Syndrome”
November 19, 2019
Emil Pajek MDCannot find the CME that is listed in the article.
ALSO the article in the magazine has DIFFERENT Title than here …cannot find the CME /article or reference.
I had to call the ACEP
February 4, 2020
David GlassSame. I can’t find the CME link / test.
March 20, 2021
J WellsI think you mean AP is diastolic pressure minus compartment pressure