Sciatica is radicular pain radiating down the buttocks along the course of the sciatic nerve. It is a common cause of low back pain, a complaint responsible for up to 2.7 million or 2.4 percent of annual United States emergency department (ED) visits.1, 2
Explore This Issue
ACEP Now: Vol 41 – No 06 – June 2022Typically, the ED treatment of sciatica pain is limited to various analgesic regimens. Nonsteroidal anti-inflammatory drugs (NSAIDs) provide superior pain relief when compared to placebo.3 Opioids are commonly used in the treatment for sciatica, however, the long-term potential for misuse and abuse drastically decreases their utility outside of the ED.4 In addition, recent data demonstrate that a single dose of opioids in the ED is not superior to alternatives.5 With such limited options for managing acute pain, additional modalities are needed.
The ultrasound-guided transgluteal sciatic nerve block (TGSNB)—a relatively new block—was first described in 2019 in emergency medicine literature as an analgesic technique for radicular sciatic pain.6 The TGSNB targets the sciatic nerve in the proximal leg leading to radicular pain relief. Although commonly used in anesthesia literature for orthopedic and podiatry surgeries, TGSNB utilization was uncommon until a recent case series demonstrated its superior pain relief in acute sciatica.6 Given the high volume of patients with sciatica in the ED, the TGSNB offers a highly effective or adjunctive pain treatment modality for many ED patients.
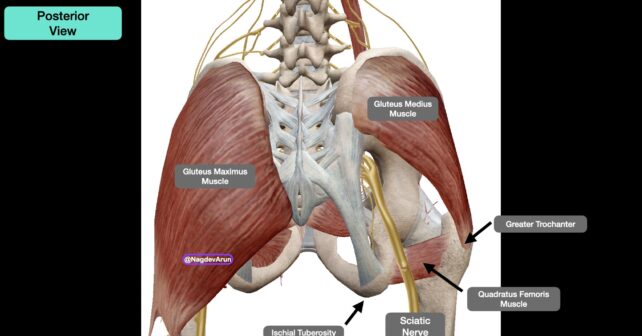
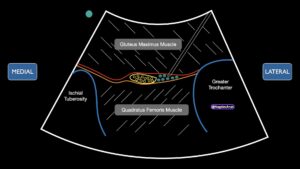
PICTURE 1 (click to enlarge): Anatomy image from the posterior view with relevant anatomy. On the right side, the gluteus maximus is left intact. On the right, the gluteus maximus has been removed so that the sciatic nerve can be clearly visualized running above the quadratus femoris muscle, and between the great trochanter (lateral) and ischial tuberosity (medial).
Anatomy and Innervation
The TGSNB targets the sciatic nerve at the level of the greater trochanter. Anatomically, the sciatic nerve is identified inferior to the gluteus maximus muscle as it courses adjacent to the ischial tuberosity (medially) and greater trochanter (laterally) (Picture 1). The sciatic nerve provides sensory innervation to the skin of the lower foot and lower leg. The medial aspect of the lower leg is innervated by the saphenous nerve. The peroneal branch of the sciatic nerve provides motor innervation to the muscles that dorsiflex the foot. As we are providing anesthetic proximally, one potential temporary side effect of the TGSNB is a foot drop.
Supplies
- Low-frequency curvilinear transducer (5–1 MHz) allows for greater visualization of the sciatic nerve and surrounding landmarks given their depth. In thin patients, and when learning to locate relevant anatomy, a high frequency linear transducer may be used (13–6 MHz).
- Anesthetic: 10 ml of 0.5 percent bupivacaine (5 mg/mL; maximum 2 mg/kg). Optional: 4–8 mg of dexamethasone may be added to increase half life of the bupivacaine.
- One 10 cc normal saline flush to hydro-dissect the sciatic nerve away from the gluteus maximus.
- 100 mm 21 gauge blunt-tip block needle or 20–22 gauge Quinke spinal needle (90 mm). Needle visualization for deep target blocks is significantly easier when using echogenic block needles.
- 91 cm or 36 inch tubing (if not using a block needle).
- Chlorhexidine skin prep.
- Transparent dressing (Tegaderm) for the transducer and sterile gel-packets.
- 25–30 g needle for local skin wheal.
Procedure
1. Pre-block
The clinician should be knowledgeable of the signs, symptoms, and treatment of local anesthetic systemic toxicity (LAST) and have 20 percent lipid emulsion therapy readily available for this rare but potentially serious complication. We recommend placing the patient on a monitor.
2. Positioning
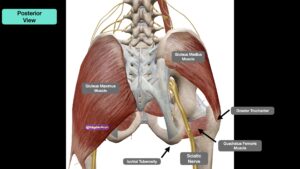
PICTURE 2A (click to enlarge): Place the patient in a lateral position, if possible, with mild knee flexion. Note the probe (red oval) with the probe marker (green circle) pointed to the ischial tuberosity (medial). PICTURE 2B (click to enlarge): Representative anatomy when placing the ultrasound transducer in between the greater trochanter and ischial tuberosity. Note the inplane lateral to medial needle approach in the top image. Also, note the quadratus femoris muscle (blue star). Green circle indicates probe marker.
The patient’s proximal affected leg should be exposed. The patient should be in a lateral decubitus position with the affected side up and the knee flexed at a 90 degree angle. The ultrasound machine should be placed so that the clinician can look directly at the screen as well as the site of needle entry in the same line of sight (Pictures 2A and 2B).
3. Procedure Details
With the patient in the lateral decubitus position, palpate for the greater trochanter laterally and the posterior superior iliac spine medially. A line between the two landmarks will indicate the path of the needle. A curvilinear probe (1–5 MHz) should be placed along this line.
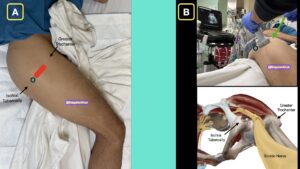
PICTURE 3A (click to enlarge): Ultrasound image for the TGSNB. Note the greater trochanter and ischial tuberosity. The sciatic nerve is located in the fascial planes between the gluteus maximus muscle (superficially) and the quadratus femoris muscle (deeper). PICTURE 3B (click to enlarge): Schematic representation of the ultrasound image.
The greater trochanter will be located laterally and the ischial tuberosity should be located medially identified as hyperechoic structures on the screen. In some patients, the ischial tuberosity will be hard to identify. The sciatic nerve will appear as a flattened, round or triangular hyperechoic structure lying within the fascial plane between the gluteus maximus and quadratus femoris muscles. It will usually be located about 4–6 cm below the skin. (Pictures 3A and 3B)
If having difficulty identifying the sciatic nerve at this level, you can also identify the distal sciatic nerve in the mid to distal posterior thigh and follow the nerve proximally to the level of the ischial tuberosity and greater trochanter. This video explains how to perform an ultrasound-guided distal sciatic nerve block in the popliteal fossa: https://www.acepnow.com/multimedia/ultrasound-guided-distal-sciatic-nerve-block/.
4. Skin Wheal
After satisfactory identification of the proximal sciatic nerve, widely prep the skin with chlorhexidine, allow to completely dry, and place 2–3 mL lidocaine skin wheal, 2–3 cm cephalad, or caudad to the transducer. The site can be either cephalad or caudad to the probe as the sciatic nerve can be approached from either direction. After sterile prep, place a lidocaine skin wheal at the insertion site using a 27 gauge needle.
5. Needle Entry
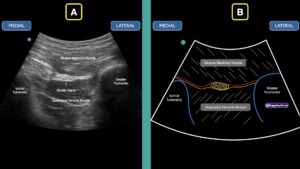
PICTURE 4 (click to enlarge): Schematic of an in-plane lateral to medial approach with a blunt block needle. Note that the anesthetic is placed in the fascial plane adjacent to the sciatic nerve. Note the nerve encompasses the yellow circles and the anesthetic is the green/blue circles.
With the transducer fixed over the targeted nerve, using an in-plane approach, insert a block needle and/or blunt tip needle and advance at approximately 70 degrees from the greater trochanter down toward the sciatic nerve (Picture 4). After the 1–2 cm of insertion, stop further needle advancement and make subtle probe adjustments until the needle is visualized. Continue advancing with in-plane ultrasound guidance to position the needle tip approximately 1–2 cm away from the nerve. Once the needle tip is visualized adjacent to the sciatic nerve, aspirate prior to injecting small aliquots of sterile saline to hydro-dissect the gluteal maximus fascial plane. Anechoic fluid should be seen separating the fascial plane away from the sciatic nerve.(Picture 4) After aspiration to ensure no vascular puncture, small aliquots of anesthetic are first injected deep to the sciatic nerve followed by the medial aspect of the nerve. Afterwards, advance the needle to the far side of the nerve, aspirate to ensure no vascular puncture, and inject small aliquots of anesthetic on the far side then the proximal aspect of the nerve. In our experience, this order of injection helps prevent any obscuring of the nerve of interest in case there is a small amount of air that was not fully expressed from the needle or tubing prior to initiating the procedure. Ensure that the injected anechoic fluid is not placed in the gluteus maximus muscle or into the sciatic nerve itself.
Summary
The TGSNB is a simple, safe block that can provide pain relief to a large number of patients in your ED. Given its effectiveness, this can be a valuable tool for acute multimodal pain control for a condition that usually can be difficult to manage with traditional oral analgesics. The combination of dexamethasone to a long-acting anesthetic may provide longer pain relief and further provide additional time for your patient to get ahead of their pain cycle.
Andrew J Goldsmith, MD, MBA, is Ultrasound director at Brigham and Women’s Hospital
Joseph Brown, MD, is a part of the Ultrasound Division at the University of Colorado.
Jeff Herrala, MD, is a resident physician at Highland Hospital.
Arun Nagdev, MD, is director of the Ultrasound Division at Highland Hospital
References
- Friedman BW, Chilstrom M, Bijur PE, Gallaghar EJ. Diagnostic testing and treatment of low back pain in United States emergency departments: a national perspective. Spine (Phila Pa 1976). 2010;35(24):E1406–11. https://doi.org/10.1097/BRS. 0b013e3181d952a5.
- Friedman BW, O’Mahony S, Mulvey L, et al. One-week and 3-month outcomes after an emergency department visit for undifferentiated musculoskeletal low back pain. Ann Emerg Med. 2012;59(2):128–133.e3. https://doi.org/10.1016/j.annemergmed. 2011.09.012.
- Enthoven W, Roelofs P, Deyo R, van Tulder MW, Koes BW. Non-steroidal antiinflammatory drugs for chronic low back pain. Cochrane Database Syst Rev. 2016;2 (2). https://doi.org/10.1002/14651858.CD012087 CD012087. Published 2016 Feb 10.
- Hooten WM, Cohen SP. Evaluation and treatment of low back pain: a clinically focused review for primary care specialists. Mayo Clin Proc. 2015;90(12):1699–718. https://doi.org/10.1016/j.mayocp.2015.10.009.
- Chang AK, Bijur PE, Esses D, Barnaby DP, Baer J. Effect of a single dose of oral opioid and nonopioid analgesics on acute extremity pain in the emergency department: a randomized clinical trial. JAMA. 2017;318(17):1661–7. https://doi.org/10.1001/ jama.2017.16190.
- Goldsmith, Andrew J., et al. “Ultrasound-Guided Transgluteal Sciatic Nerve Analgesia for Refractory Back Pain in the Ed.” The American Journal of Emergency Medicine, vol. 38, no. 9, 2020, pp. 1792–1795. https://doi.org/10.1016/j.ajem.2020.06.001.
Pages: 1 2 3 4 | Multi-Page





No Responses to “How To Relieve Sciatica Pain with New TransGluteal Nerve Block Treatment”