Geriatric emergency medicine (GEM) is an area of growing importance within emergency medicine. The population of adults age 65 and older in the United States increased from 31 million in 1990 to 40 million in 2010, and it is projected to increase to more than 70 million in 2030 (see Figure 1).1,2
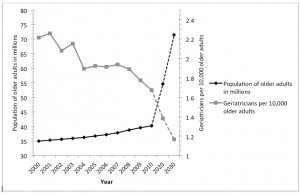
Figure 1. Population estimates for the number of older adults and geriatricians per 10,000 older adults in the United States by 2030.
Both the absolute number and the proportion of emergency department visits by older adults are rising.3 In order to respond to the needs of this population, more emergency physicians with proficiency in GEM are needed, and fellowship training is one pathway to expertise for physicians with an interest in the field.
GEM Training from Medical School to Fellowship and Beyond
Educational guidelines in geriatrics have been developed for medical students, EM residents, and fellows.4-6 For medical students, there are 26 defined competencies in geriatric care, including evaluation of cognitive and behavioral disorders, health care planning, medication management, atypical presentations of diseases, palliative care, and the effect of comorbid conditions.4 For EM residents, there are established GEM competencies.5 Interactive curricula (published with open access online at POGOe and MedEdPortal) have been developed, and their use has been correlated with improved care.7-9
For more advanced training, fellowships in GEM are available at four institutions, and more institutions likely will start fellowship programs in the near future.10 The first program began in 2001, and active programs currently exist at the William Beaumont Hospital in Royal Oak, Mich; NewYork-Presbyterian Hospital; the University of North Carolina at Chapel Hill; and the University of California, Davis (see “The UC Davis Geriatric Emergency Medicine Fellowship Program: Nuts and Bolts” for more on UC Davis’s program).
While understanding the subtleties of diagnosing and treating older adults is certainly within the purview of all emergency physicians, GEM fellowships provide additional training to prepare physicians to be leaders in the field, setting up clinical protocols for their EDs, developing and performing research in elder care, creating educational programs focusing on the care of older adults in the ED, and generally helping the field of EM evolve toward more gero-sensitive care.
GEM fellowships are one- or two-year, non-ACGME-accredited post-residency training positions. Fellowships typically involve close collaboration with existing, well-established fellowship programs in geriatric internal medicine. Fellows are exposed to the care of elderly patients in a range of settings including the ED, primary and specialty care clinics, inpatient and intensive care units, long-term care and skilled nursing facilities, palliative care services, and hospice environments. The Society for Academic Emergency Medicine fellowship guidelines include 12 core components of expertise in clinical care that all fellows should master:
- Atypical presentations of disease in older adults
- Trauma and falls
- Cognitive and behavioral disorders
- Emergency intervention modifications
- Medication management
- Transitions of care
- Effect of comorbid conditions
- Ethics, palliative care, and end-of-life issues
- Continuum of care
- Geriatric syndromes
- Wound management/pressure ulcers
- End-of-life care
In addition to mastering the clinical components, fellows are expected to excel and meet additional competencies in education, administration, or research.
As the number of ED visits by older adults continues to grow, all emergency physicians will need to become more aware of the challenges involved in their care, from diagnosis, disease management, and recognition of geriatric syndromes to safe discharge and the development of systems of care. Because GEM is a young and rapidly growing discipline, there is great potential for physicians who become involved in GEM or pursue GEM fellowships to have a significant impact on the field and on the future ED care of older adults.
References
1. U.S. Census Bureau statistical abstract of the United States: 2012. Resident population by sex and age: 1980 to 2010. U.S. Census Bureau Web site. Available at: http://www.census.gov/compendia/statab/2012/tables/12s0007.pdf. Accessed July 31, 2013.
2. Committee on the Future Health Care Workforce for Older Americans, Institute of Medicine. Retooling for an aging America: building the health care workforce. 1st ed. Washington, DC: National Academic Press; 2008:316.
3. Roberts DC, McKay MP, Shaffer A. Increasing rates of emergency department visits for elderly patients in the United States, 1993 to 2003. Ann Emerg Med. 2008;51:769-774.
4. Leipzig RM, Granville L, Simpson D, et al. Keeping granny safe on July 1: A consensus on minimum geriatrics competencies for graduating medical students. Acad Med. 2009;84:604-610.
5. Hogan TM, Losman ED, Carpenter CR, et al. Development of geriatric competencies for emergency medicine residents using an expert consensus process. Acad Emerg Med. 2010;17:316-324.
6. Society for Academic Emergency Medicine (SAEM). Application for geriatric emergency medicine fellowship.
7. POGOe. The portal of geriatrics online education. Available at: http://www.pogoe.org. Accessed August 5, 2013.
8. American Association of Medical Colleges. MedEd portal. Available at: https://www.mededportal.org. Accessed August 5, 2013.
9. Biese KJ, Roberts E, LaMantia M, et al. Effect of a geriatric curriculum on emergency medicine resident attitudes, knowledge, and decision-making. Acad Emerg Med. 2011;18 Suppl 2:S92-6.
10. Society for Academic Emergency Medicine. Fellowship directory. Available at: http://www.saem.org/membership/services/fellowship-directory. Accessed July 20, 2013.
Dr. Shenvi is a geriatric emergency medicine fellow in the Department of Emergency Medicine at the University of North Carolina (UNC), Chapel Hill. Dr. Bynum is associate professor of internal medicine, in the Division of Geriatrics at UNC. Dr. Biese is associate professor of emergency medicine at USC.
Pages: 1 2 | Multi-Page





No Responses to “Geriatic Emergency Medicine Training Valued as More Seniors Visit the ED”